While we try to keep things accurate, this content is part of an ongoing experiment and may not always be reliable.
Please double-check important details — we’re not responsible for how the information is used.
Cancer
Revolutionizing Quantum Communication: Direct Connections Between Multiple Processors
Researchers developed a scalable interconnect that facilitates all-to-all communication among many quantum processor modules by enabling each to send and receive quantum information on demand in a user-specified direction. They used the interconnect to demonstrate remote entanglement, a type of correlation that is key to creating a powerful, distributed network of quantum processors.

Cancer
A Silent Killer Unmasked: The Hidden Gene in Leukemia Virus that Could Revolutionize HIV Treatment
Scientists in Japan have discovered a genetic “silencer” within the HTLV-1 virus that helps it stay hidden in the body, evading the immune system for decades. This silencer element essentially turns the virus off, preventing it from triggering symptoms in most carriers. Incredibly, when this silencer was added to HIV, it made that virus less active too — hinting at a revolutionary new strategy for managing not just HTLV-1 but other deadly retroviruses as well. The discovery opens the door to turning the virus’s own stealth tactics against it in future treatments.
Cancer
Turning Yogurt into a Healing Gel: Columbia Scientists Pioneer New Regenerative Medicine Approach
Scientists at Columbia Engineering have developed an injectable hydrogel made from yogurt-derived extracellular vesicles (EVs) that could revolutionize regenerative medicine. These EVs serve both as healing agents and as structural components, eliminating the need for added chemicals. The innovation leverages everyday dairy products like yogurt to create a biocompatible material that mimics natural tissue and enhances healing.
Cancer
Safer Non-Stick Coatings: Scientists Develop Alternative to Teflon
Scientists at the University of Toronto have developed a new non-stick material that rivals the performance of traditional PFAS-based coatings while using only minimal amounts of these controversial “forever chemicals.” Through an inventive process called “nanoscale fletching,” they modified silicone-based polymers to repel both water and oil effectively. This breakthrough could pave the way for safer cookware, fabrics, and other products without the environmental and health risks linked to long-chain PFAS.
-

 Detectors10 months ago
Detectors10 months agoA New Horizon for Vision: How Gold Nanoparticles May Restore People’s Sight
-

 Earth & Climate11 months ago
Earth & Climate11 months agoRetiring Abroad Can Be Lonely Business
-

 Albert Einstein11 months ago
Albert Einstein11 months agoHarnessing Water Waves: A Breakthrough in Controlling Floating Objects
-

 Chemistry10 months ago
Chemistry10 months ago“Unveiling Hidden Patterns: A New Twist on Interference Phenomena”
-

 Earth & Climate10 months ago
Earth & Climate10 months agoHousehold Electricity Three Times More Expensive Than Upcoming ‘Eco-Friendly’ Aviation E-Fuels, Study Reveals
-

 Agriculture and Food11 months ago
Agriculture and Food11 months ago“A Sustainable Solution: Researchers Create Hybrid Cheese with 25% Pea Protein”
-

 Diseases and Conditions11 months ago
Diseases and Conditions11 months agoReducing Falls Among Elderly Women with Polypharmacy through Exercise Intervention
-

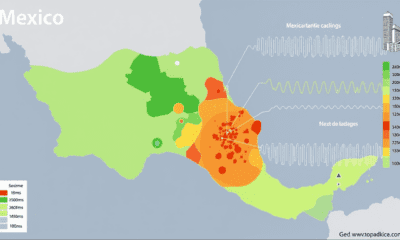
 Earth & Climate11 months ago
Earth & Climate11 months agoPredicting Damage from Local Earthquakes in Mexico City