While we try to keep things accurate, this content is part of an ongoing experiment and may not always be reliable.
Please double-check important details — we’re not responsible for how the information is used.
Chronic Illness
Revolutionizing Heart Disease Screening with a Handheld Device
Researchers have developed a handheld device that could potentially replace stethoscopes as a tool for detecting certain types of heart disease.

Allergy
The Resilient Enemy: Why Asthma Symptoms Persist Despite Powerful Drugs
Biological drugs have been a game-changer for people with severe asthma, helping them breathe easier and live more comfortably. But researchers at Karolinska Institutet have uncovered a surprising twist: while these treatments ease symptoms, they may not fully eliminate the immune cells that drive inflammation. In fact, some of these cells actually increase during treatment, suggesting the medication is managing symptoms without targeting the root cause. This could explain why asthma often returns when the drugs are stopped, raising questions about how long-term these treatments should be and whether we’re truly solving the underlying problem.
Animal Learning and Intelligence
“Breathe with Identity: The Surprising Link Between Your Breath and You”
Scientists have discovered that your breathing pattern is as unique as a fingerprint and it may reveal more than just your identity. Using a 24-hour wearable device, researchers achieved nearly 97% accuracy in identifying people based solely on how they breathe through their nose. Even more intriguingly, these respiratory signatures correlated with traits like anxiety levels, sleep cycles, and body mass index. The findings suggest that breathing isn t just a passive process it might actively shape our mental and emotional well-being, opening up the possibility of using breath training for diagnosis and treatment.
Chronic Illness
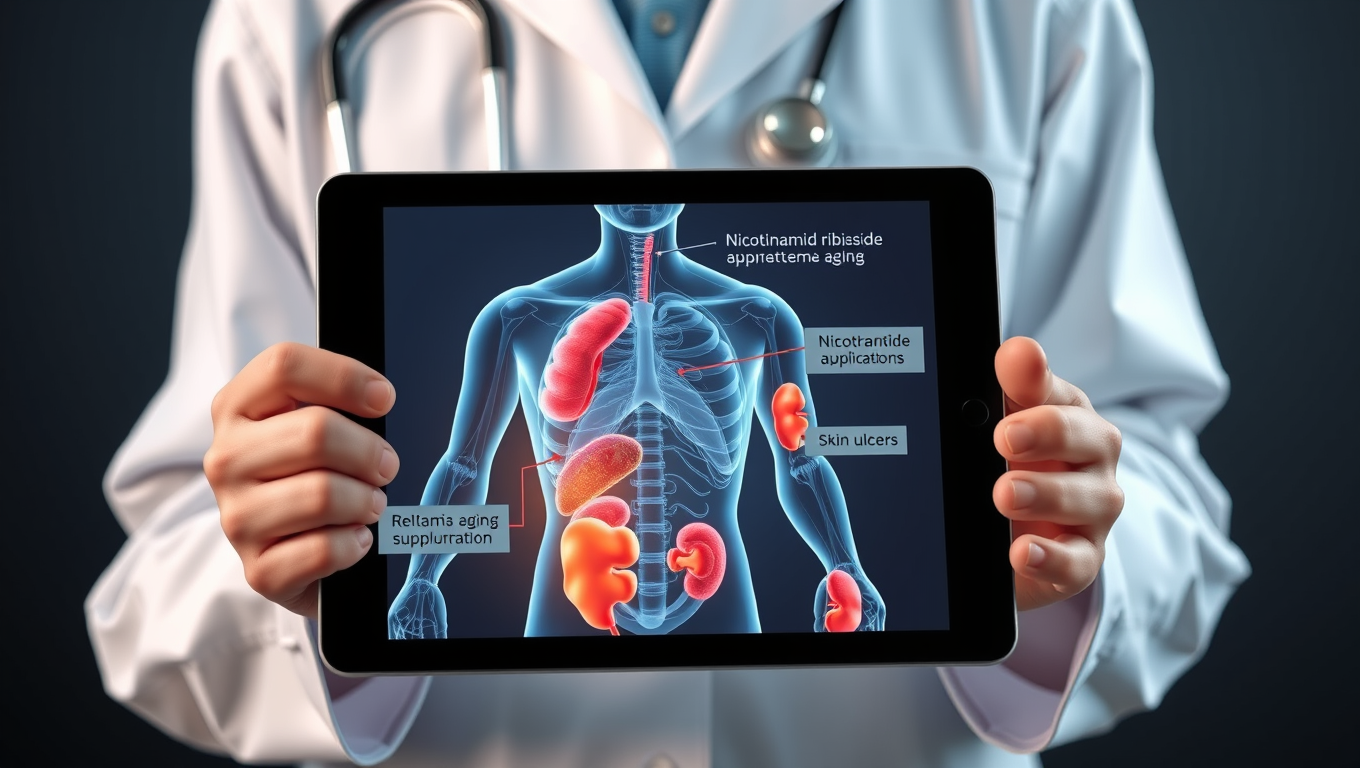
Groundbreaking Supplement Reverses Premature Aging in Landmark Human Trial
A rare genetic disorder called Werner syndrome causes premature aging and devastating health complications from an early age, yet treatment options have been lacking. New hope emerges from Chiba University, where researchers conducted the first clinical trial using nicotinamide riboside (NR), a precursor to NAD+ that s been linked to anti-aging effects. The double-blind trial revealed that NR not only safely boosted NAD+ levels but also improved cardiovascular health, reduced skin ulcers, and helped protect kidney function in patients.
-

 Detectors3 months ago
Detectors3 months agoA New Horizon for Vision: How Gold Nanoparticles May Restore People’s Sight
-

 Earth & Climate4 months ago
Earth & Climate4 months agoRetiring Abroad Can Be Lonely Business
-

 Cancer3 months ago
Cancer3 months agoRevolutionizing Quantum Communication: Direct Connections Between Multiple Processors
-

 Agriculture and Food4 months ago
Agriculture and Food4 months ago“A Sustainable Solution: Researchers Create Hybrid Cheese with 25% Pea Protein”
-

 Diseases and Conditions4 months ago
Diseases and Conditions4 months agoReducing Falls Among Elderly Women with Polypharmacy through Exercise Intervention
-

 Chemistry3 months ago
Chemistry3 months ago“Unveiling Hidden Patterns: A New Twist on Interference Phenomena”
-

 Albert Einstein4 months ago
Albert Einstein4 months agoHarnessing Water Waves: A Breakthrough in Controlling Floating Objects
-

 Earth & Climate3 months ago
Earth & Climate3 months agoHousehold Electricity Three Times More Expensive Than Upcoming ‘Eco-Friendly’ Aviation E-Fuels, Study Reveals