While we try to keep things accurate, this content is part of an ongoing experiment and may not always be reliable.
Please double-check important details — we’re not responsible for how the information is used.
Diseases and Conditions
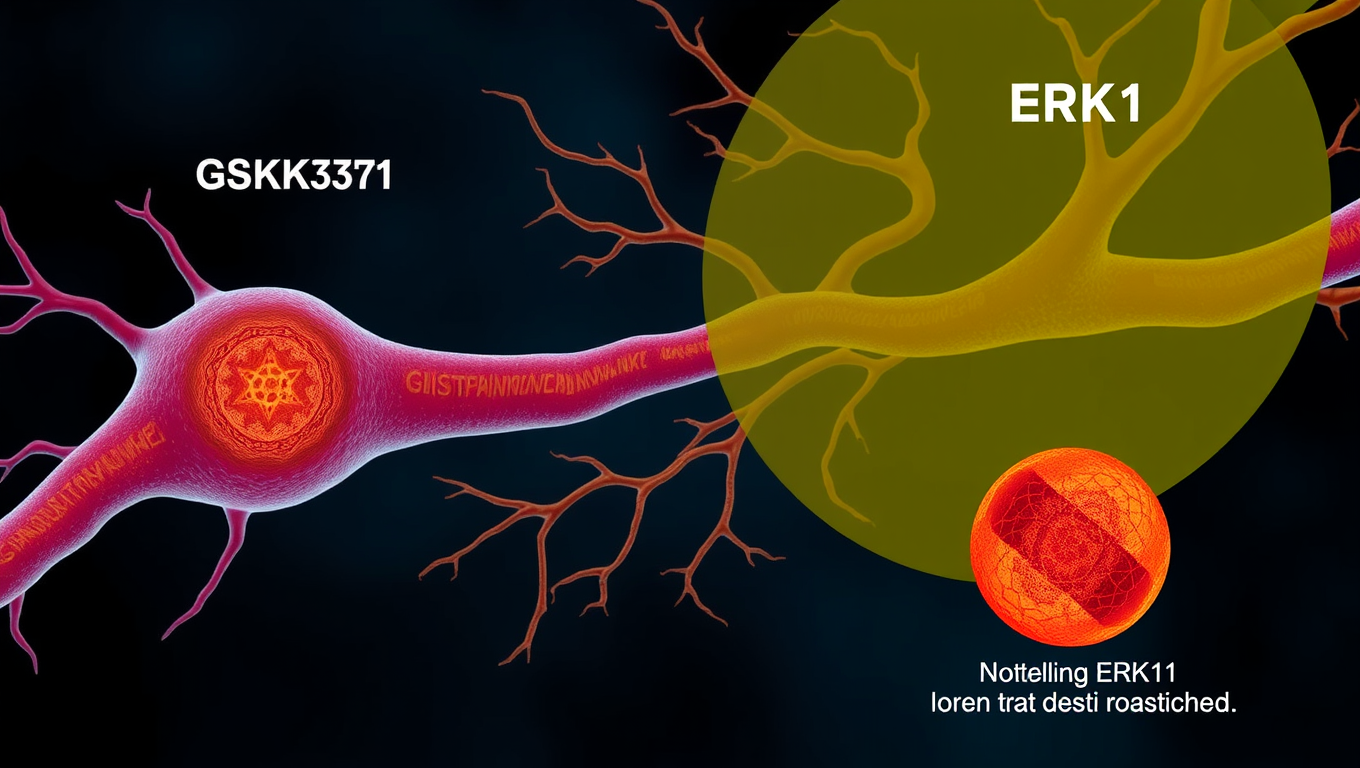
Unlocking the Secrets of Huntington’s Disease: Two Proteins with Opposing Effects
Researchers found that inhibiting GSK-3 led to less defects in the axonal transport process and less neuronal cell death, while inhibiting ERK1 led to more transport problems and more cell death.
Diseases and Conditions
Mapping Immunity: Breaking Down the Barriers to Pig-to-Human Transplants
Scientists have achieved an unprecedented look into how the human immune system attacks a transplanted pig kidney, using spatial molecular imaging to map immune activity down to the cellular level. They discovered early signs of rejection within 10 days and pinpointed key immune players—like macrophages—driving the response. Even more exciting: when targeted therapies were applied, the immune assault weakened. As U.S. clinical trials of pig kidney transplants begin, this breakthrough offers hope for overcoming the immune barrier that has long stood in the way of xenotransplantation.
Diseases and Conditions
Uncovering CMV’s Secret Weapon: A Breakthrough in Developing Therapy Against a Leading Cause of Birth Defects
Scientists have discovered a stealthy mechanism that cytomegalovirus (CMV)—the leading infectious cause of birth defects in the U.S.—uses to infiltrate blood vessel cells while evading immune detection. The virus forms a hidden protein complex that acts like a molecular “backdoor,” allowing it to bypass the immune system’s defenses. This newly identified pathway may explain why vaccine efforts have failed for decades and opens the door to targeted therapies that could finally prevent CMV-linked birth defects in newborns and protect vulnerable patients.
Cancer
A Breakthrough in Inflammation Control: Scientists Discover ‘Off Switch’ Enzyme to Combat Heart Disease and Diabetes
Researchers at UT Arlington have discovered a key enzyme, IDO1, that when blocked, helps immune cells regain their ability to properly process cholesterol—something that breaks down during inflammation. This breakthrough could offer a powerful new way to fight heart disease, diabetes, cancer, and more. By “turning off” this enzyme, the team restored cholesterol absorption in macrophages, potentially stopping disease at the source. Even more promising, they found a second enzyme, NOS, that makes things worse—raising hopes that targeting both could pave the way for transformative treatments for millions suffering from inflammation-driven conditions.
-

 Detectors3 months ago
Detectors3 months agoA New Horizon for Vision: How Gold Nanoparticles May Restore People’s Sight
-

 Earth & Climate4 months ago
Earth & Climate4 months agoRetiring Abroad Can Be Lonely Business
-

 Cancer3 months ago
Cancer3 months agoRevolutionizing Quantum Communication: Direct Connections Between Multiple Processors
-

 Agriculture and Food3 months ago
Agriculture and Food3 months ago“A Sustainable Solution: Researchers Create Hybrid Cheese with 25% Pea Protein”
-

 Diseases and Conditions4 months ago
Diseases and Conditions4 months agoReducing Falls Among Elderly Women with Polypharmacy through Exercise Intervention
-

 Chemistry3 months ago
Chemistry3 months ago“Unveiling Hidden Patterns: A New Twist on Interference Phenomena”
-

 Albert Einstein4 months ago
Albert Einstein4 months agoHarnessing Water Waves: A Breakthrough in Controlling Floating Objects
-

 Earth & Climate3 months ago
Earth & Climate3 months agoHousehold Electricity Three Times More Expensive Than Upcoming ‘Eco-Friendly’ Aviation E-Fuels, Study Reveals