While we try to keep things accurate, this content is part of an ongoing experiment and may not always be reliable.
Please double-check important details — we’re not responsible for how the information is used.
Chronic Illness
Unlocking the Secrets of Kidney Scarring: A Precision Medicine Approach to Prevent Chronic Kidney Disease Progression
Researchers have identified type 5 collagen as a key factor in kidney fibrosis, revealing its potential as a biomarker to predict chronic kidney disease progression. A repurposed anti-cancer drug, Cilengitide, was found to reduce kidney scarring and slow disease progression in preclinical models, suggesting a possible precision medicine approach for high-risk patients. The team now seeks to develop a blood test to measure type 5 collagen levels, which could help identify patients at greater risk for kidney failure and guide targeted treatment strategies.
Chronic Illness
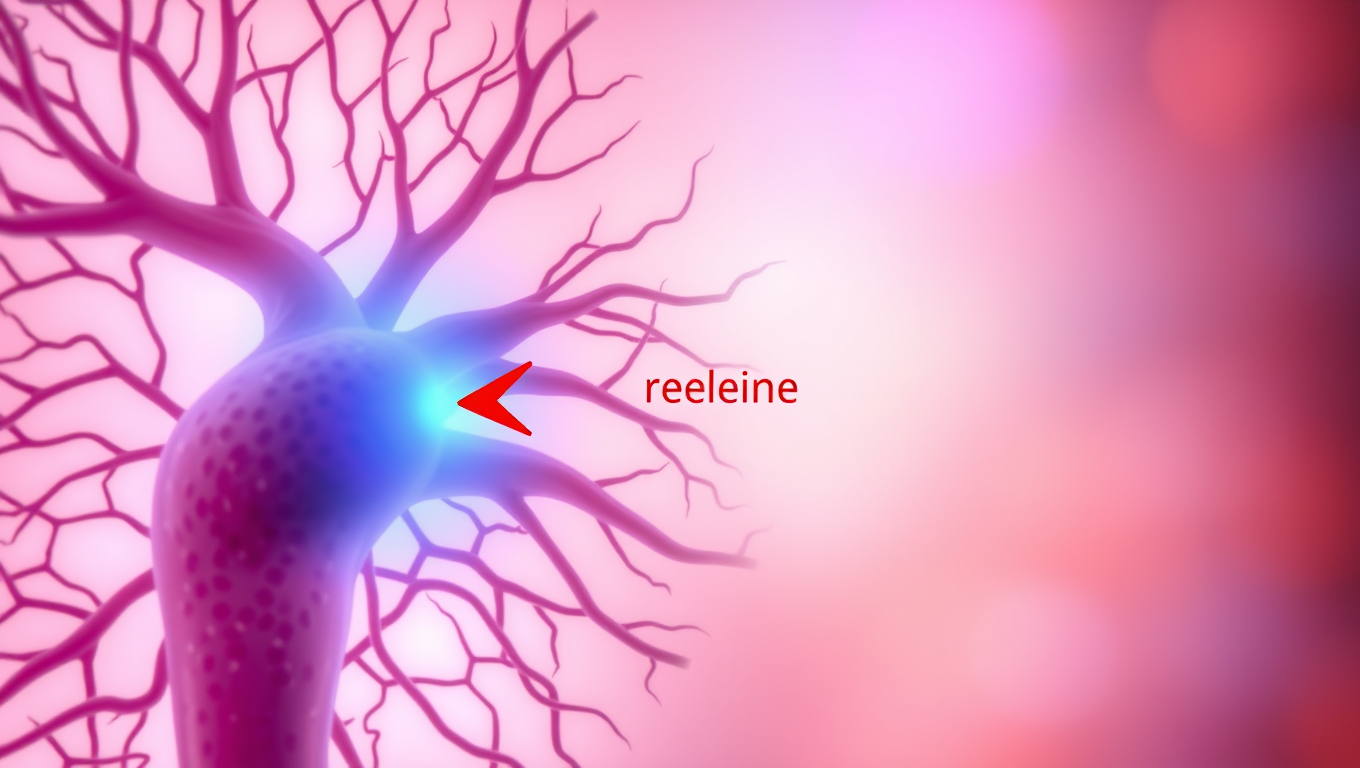
Scientists Uncover Hidden Brain Shortcut for Weight Loss without Nausea
Scientists have uncovered a way to promote weight loss and improve blood sugar control without the unpleasant side effects of current GLP-1 drugs. By shifting focus from neurons to brain support cells that produce appetite-suppressing molecules, they developed a modified compound, TDN, that worked in animal tests without causing nausea or vomiting.
Cancer
A Silent Killer Unmasked: The Hidden Gene in Leukemia Virus that Could Revolutionize HIV Treatment
Scientists in Japan have discovered a genetic “silencer” within the HTLV-1 virus that helps it stay hidden in the body, evading the immune system for decades. This silencer element essentially turns the virus off, preventing it from triggering symptoms in most carriers. Incredibly, when this silencer was added to HIV, it made that virus less active too — hinting at a revolutionary new strategy for managing not just HTLV-1 but other deadly retroviruses as well. The discovery opens the door to turning the virus’s own stealth tactics against it in future treatments.
Chronic Illness
The Hidden Link Between Sleep Schedule and Disease Risk
A global study of over 88,000 adults reveals that poor sleep habits—like going to bed inconsistently or having disrupted circadian rhythms—are tied to dramatically higher risks for dozens of diseases, including liver cirrhosis and gangrene. Contrary to common belief, sleeping more than 9 hours wasn’t found to be harmful when measured objectively, exposing flaws in previous research. Scientists now say it’s time to redefine “good sleep” to include regularity, not just duration, as biological mechanisms like inflammation may underlie these powerful sleep-disease links.
-

 Detectors11 months ago
Detectors11 months agoA New Horizon for Vision: How Gold Nanoparticles May Restore People’s Sight
-

 Earth & Climate12 months ago
Earth & Climate12 months agoRetiring Abroad Can Be Lonely Business
-

 Cancer11 months ago
Cancer11 months agoRevolutionizing Quantum Communication: Direct Connections Between Multiple Processors
-

 Albert Einstein12 months ago
Albert Einstein12 months agoHarnessing Water Waves: A Breakthrough in Controlling Floating Objects
-

 Chemistry11 months ago
Chemistry11 months ago“Unveiling Hidden Patterns: A New Twist on Interference Phenomena”
-

 Earth & Climate11 months ago
Earth & Climate11 months agoHousehold Electricity Three Times More Expensive Than Upcoming ‘Eco-Friendly’ Aviation E-Fuels, Study Reveals
-

 Agriculture and Food11 months ago
Agriculture and Food11 months ago“A Sustainable Solution: Researchers Create Hybrid Cheese with 25% Pea Protein”
-

 Diseases and Conditions12 months ago
Diseases and Conditions12 months agoReducing Falls Among Elderly Women with Polypharmacy through Exercise Intervention