While we try to keep things accurate, this content is part of an ongoing experiment and may not always be reliable.
Please double-check important details — we’re not responsible for how the information is used.
Cosmetic Surgery
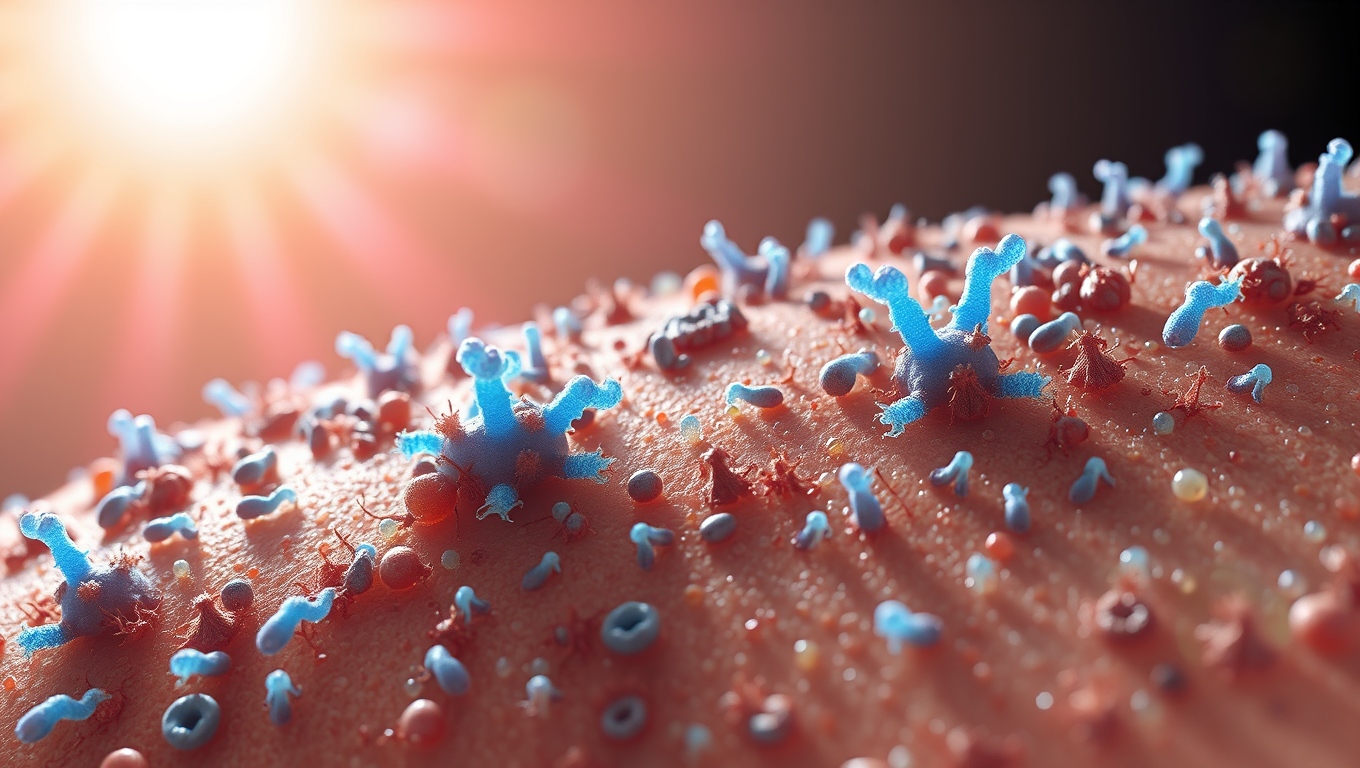
“Microbes on Our Skin: The Hidden Heroes Against Sun Damage”
The skin microbiome plays an important role in health and disease. Researchers have now substantiated that certain skin bacteria can protect us from the sun’s ultraviolet (UV) radiation specifically by metabolizing cis-urocanic acid using an enzyme called urocanase. This enables the skin’s ability to fine-tune how it responds to UV radiation. The findings demonstrate the ability of the skin microbiome to remodel host immune functions.
Alternative Medicine
“Skin in a Syringe”: Breakthrough Technology Heals Burns without Scars
Scientists in Sweden have developed a groundbreaking “skin in a syringe” — a gel packed with live cells that can be applied directly to wounds or even 3D-printed into skin grafts. Designed to help the body build functional dermis rather than scar tissue, the innovation combines fibroblast cells on gelatin beads with a hyaluronic acid gel, held together using click chemistry. In a parallel advance, the team also created elastic hydrogel threads that can form tiny, fluid-carrying channels, paving the way for artificial tissues and organoid development.
Alternative Medicine
Patients Who Undergo Tummy Tuck Surgery Continue to Lose Weight Years Later, Study Finds
Patients who undergo tummy tuck surgery may be in for more than just cosmetic changes — a new study shows they often keep losing weight for years after the procedure. Researchers followed 188 patients and found consistent weight reduction up to five years later, especially in those with higher initial BMIs. Interestingly, lifestyle improvements, such as better diet and exercise habits, may play a key role in this surprising long-term effect. This could mean tummy tucks aren’t just sculpting bodies — they may be reshaping lives.
Cosmetic Surgery
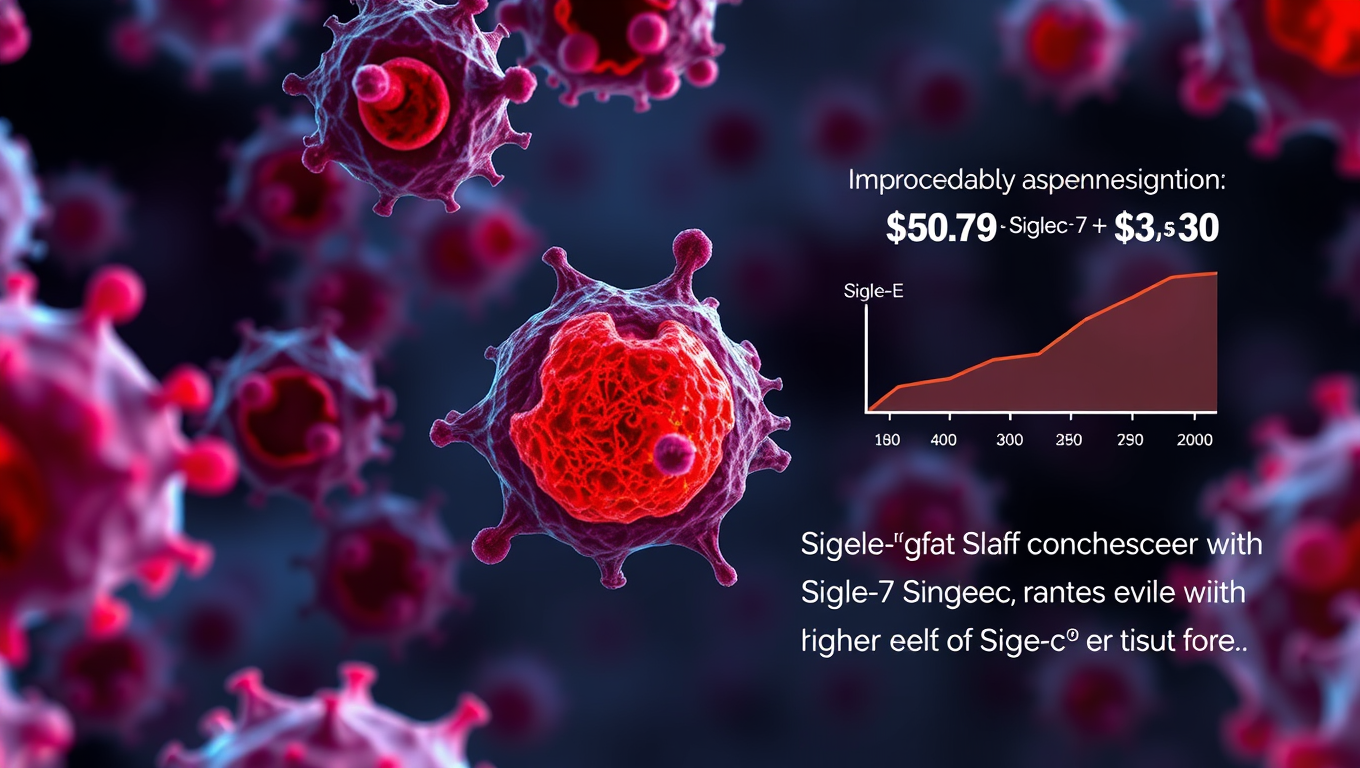
Unlocking the Innate Immune System: A New Path to Prevent Organ Transplant Rejection
Researchers identified a natural ‘brake’ within the innate immune system: the inhibitory receptor Siglec-E (SigE) and its human counterparts, Siglec-7 and Siglec-9. This receptor helps prevent overactivation of immune cells that drive rejection. When this brake is missing, inflammation worsens, leading to faster rejection in preclinical models. Importantly, transplant patients with higher levels of Siglec-7 and Siglec-9 showed better graft survival, highlighting this pathway as a promising target for new therapies.
-

 Detectors10 months ago
Detectors10 months agoA New Horizon for Vision: How Gold Nanoparticles May Restore People’s Sight
-

 Earth & Climate11 months ago
Earth & Climate11 months agoRetiring Abroad Can Be Lonely Business
-

 Cancer11 months ago
Cancer11 months agoRevolutionizing Quantum Communication: Direct Connections Between Multiple Processors
-

 Albert Einstein11 months ago
Albert Einstein11 months agoHarnessing Water Waves: A Breakthrough in Controlling Floating Objects
-

 Chemistry10 months ago
Chemistry10 months ago“Unveiling Hidden Patterns: A New Twist on Interference Phenomena”
-

 Earth & Climate10 months ago
Earth & Climate10 months agoHousehold Electricity Three Times More Expensive Than Upcoming ‘Eco-Friendly’ Aviation E-Fuels, Study Reveals
-

 Agriculture and Food11 months ago
Agriculture and Food11 months ago“A Sustainable Solution: Researchers Create Hybrid Cheese with 25% Pea Protein”
-

 Diseases and Conditions11 months ago
Diseases and Conditions11 months agoReducing Falls Among Elderly Women with Polypharmacy through Exercise Intervention