While we try to keep things accurate, this content is part of an ongoing experiment and may not always be reliable.
Please double-check important details — we’re not responsible for how the information is used.
Bacteria
New Antibiotic Breakthrough: Targeting the “Superbug” Gonorrhoea with a Novel Mechanism
Researchers discover a new class of antibiotic that selectively targets Neisseria gonorrhoeae, the bacterium that causes gonorrhoea. These substances trigger a self-destruction program, which also operates in multi-resistant variants of the pathogen.

Agriculture and Food
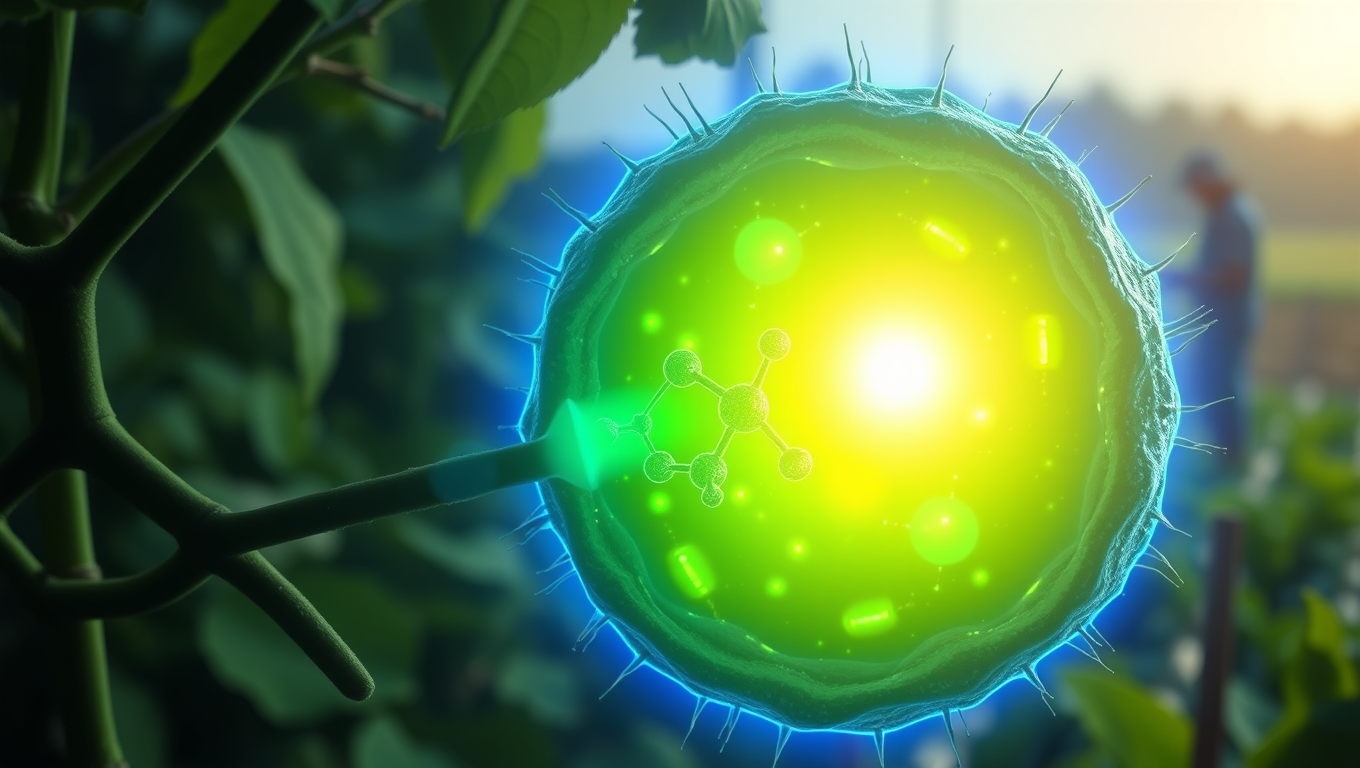
“Unlocking Photosynthesis: MIT Scientists Boost Enzyme Efficiency with Directed Evolution Technique”
Scientists at MIT have turbocharged one of nature’s most sluggish but essential enzymes—rubisco—by applying a cutting-edge evolution technique in living cells. Normally prone to wasteful reactions with oxygen, this revamped bacterial rubisco evolved to work more efficiently in oxygen-rich environments. This leap in enzyme performance could pave the way for improving photosynthesis in plants and, ultimately, increase crop yields.
Animals
“New Bat-Borne Viruses Discovered in China Pose Potential Pandemic Threat”
Two newly discovered viruses lurking in bats are dangerously similar to Nipah and Hendra, both of which have caused deadly outbreaks in humans. Found in fruit bats near villages, these viruses may spread through urine-contaminated fruit, raising serious concerns. And that’s just the start—scientists found 20 other unknown viruses hiding in bat kidneys.
Bacteria
Unveiling the Secrets of Pandoraea: How Lung Bacteria Forge Iron-Stealing Weapons to Survive
Researchers investigating the enigmatic and antibiotic-resistant Pandoraea bacteria have uncovered a surprising twist: these pathogens don’t just pose risks they also produce powerful natural compounds. By studying a newly discovered gene cluster called pan, scientists identified two novel molecules Pandorabactin A and B that allow the bacteria to steal iron from their environment, giving them a survival edge in iron-poor places like the human body. These molecules also sabotage rival bacteria by starving them of iron, potentially reshaping microbial communities in diseases like cystic fibrosis.
-

 Detectors3 months ago
Detectors3 months agoA New Horizon for Vision: How Gold Nanoparticles May Restore People’s Sight
-

 Earth & Climate4 months ago
Earth & Climate4 months agoRetiring Abroad Can Be Lonely Business
-

 Cancer4 months ago
Cancer4 months agoRevolutionizing Quantum Communication: Direct Connections Between Multiple Processors
-

 Agriculture and Food4 months ago
Agriculture and Food4 months ago“A Sustainable Solution: Researchers Create Hybrid Cheese with 25% Pea Protein”
-

 Diseases and Conditions4 months ago
Diseases and Conditions4 months agoReducing Falls Among Elderly Women with Polypharmacy through Exercise Intervention
-

 Albert Einstein4 months ago
Albert Einstein4 months agoHarnessing Water Waves: A Breakthrough in Controlling Floating Objects
-

 Chemistry3 months ago
Chemistry3 months ago“Unveiling Hidden Patterns: A New Twist on Interference Phenomena”
-

 Earth & Climate4 months ago
Earth & Climate4 months agoHousehold Electricity Three Times More Expensive Than Upcoming ‘Eco-Friendly’ Aviation E-Fuels, Study Reveals