While we try to keep things accurate, this content is part of an ongoing experiment and may not always be reliable.
Please double-check important details — we’re not responsible for how the information is used.
Disorders and Syndromes
“Placenta Plays Key Role in Genetic Risk for Schizophrenia and Other Neuropsychiatric Disorders”
An international team has identified associations between modifications in the placenta and the risk of developing schizophrenia, bipolar disorder, and major depression disorder.
Depression
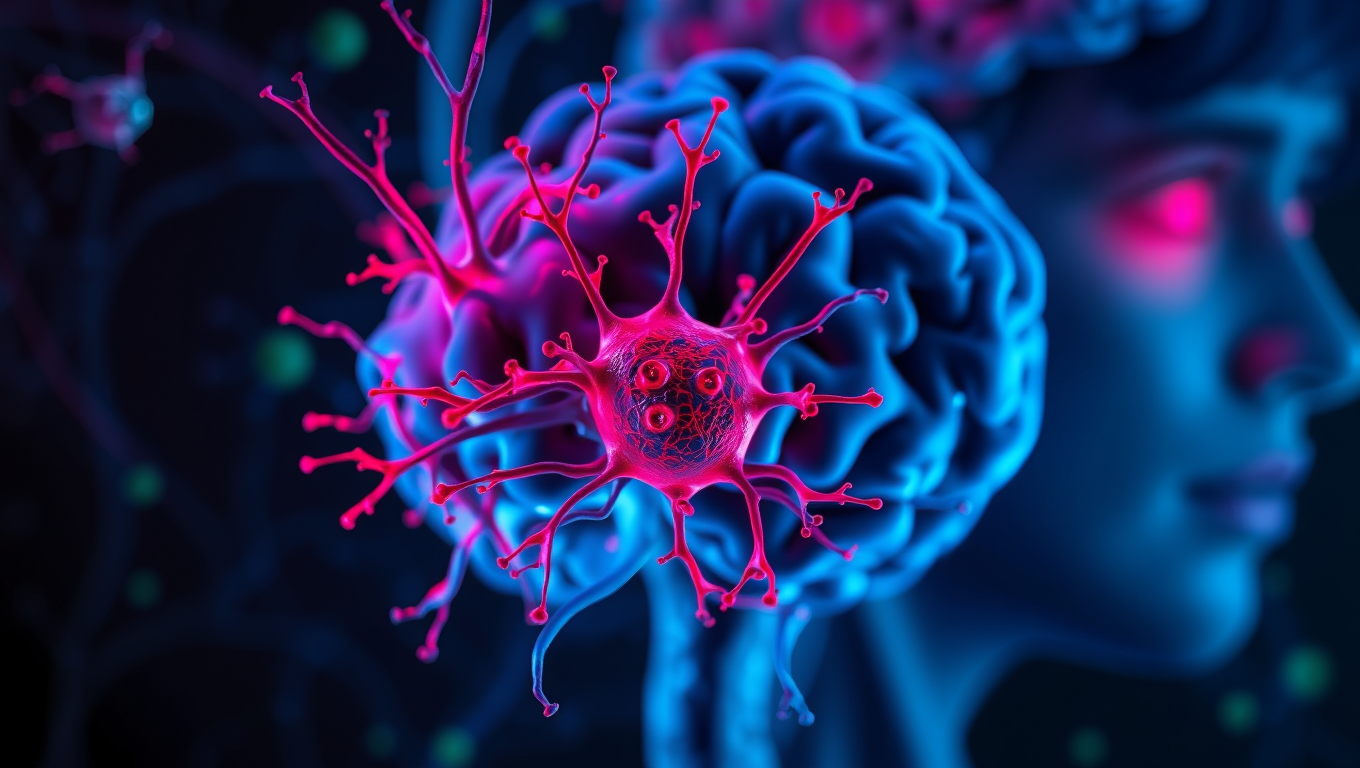
The Dark Side of Brain Cells: How They May Contribute to Depression
Major depressive disorder affects hundreds of millions worldwide, but a key to understanding its origins may lie in the brain’s immune system. New findings spotlight astrocytes—previously overshadowed by microglia—as major players in neuroinflammation that drives depression. These star-shaped brain cells, once thought to only support neurons, are now shown to regulate communication between brain cells and even trigger or amplify inflammatory responses.
Autism
CRISPR-edited stem cells hold key to understanding autism spectrum disorder
A team at Kobe University has created a game-changing resource for autism research: 63 mouse embryonic stem cell lines, each carrying a genetic mutation strongly associated with the disorder. By pairing classic stem cell manipulation with precise CRISPR gene editing, they ve built a standardized platform that mirrors autism-linked genetic conditions in mice. These models not only replicate autism-related traits but also expose key dysfunctions, like the brain s inability to clean up faulty proteins.
Diseases and Conditions
Finding the Perfect Balance: How Extra Weekend Hours Can Help Teens Manage Anxiety
Teens might finally have a good reason to sleep in on weekends within limits. A new study reveals that teenagers who get up to two extra hours of sleep on weekends show fewer anxiety symptoms than those who don t. But go beyond that sweet spot, and symptoms can actually increase.
-

 Detectors3 months ago
Detectors3 months agoA New Horizon for Vision: How Gold Nanoparticles May Restore People’s Sight
-

 Earth & Climate4 months ago
Earth & Climate4 months agoRetiring Abroad Can Be Lonely Business
-

 Cancer3 months ago
Cancer3 months agoRevolutionizing Quantum Communication: Direct Connections Between Multiple Processors
-

 Agriculture and Food4 months ago
Agriculture and Food4 months ago“A Sustainable Solution: Researchers Create Hybrid Cheese with 25% Pea Protein”
-

 Diseases and Conditions4 months ago
Diseases and Conditions4 months agoReducing Falls Among Elderly Women with Polypharmacy through Exercise Intervention
-

 Chemistry3 months ago
Chemistry3 months ago“Unveiling Hidden Patterns: A New Twist on Interference Phenomena”
-

 Albert Einstein4 months ago
Albert Einstein4 months agoHarnessing Water Waves: A Breakthrough in Controlling Floating Objects
-

 Earth & Climate3 months ago
Earth & Climate3 months agoHousehold Electricity Three Times More Expensive Than Upcoming ‘Eco-Friendly’ Aviation E-Fuels, Study Reveals