While we try to keep things accurate, this content is part of an ongoing experiment and may not always be reliable.
Please double-check important details — we’re not responsible for how the information is used.
Depression
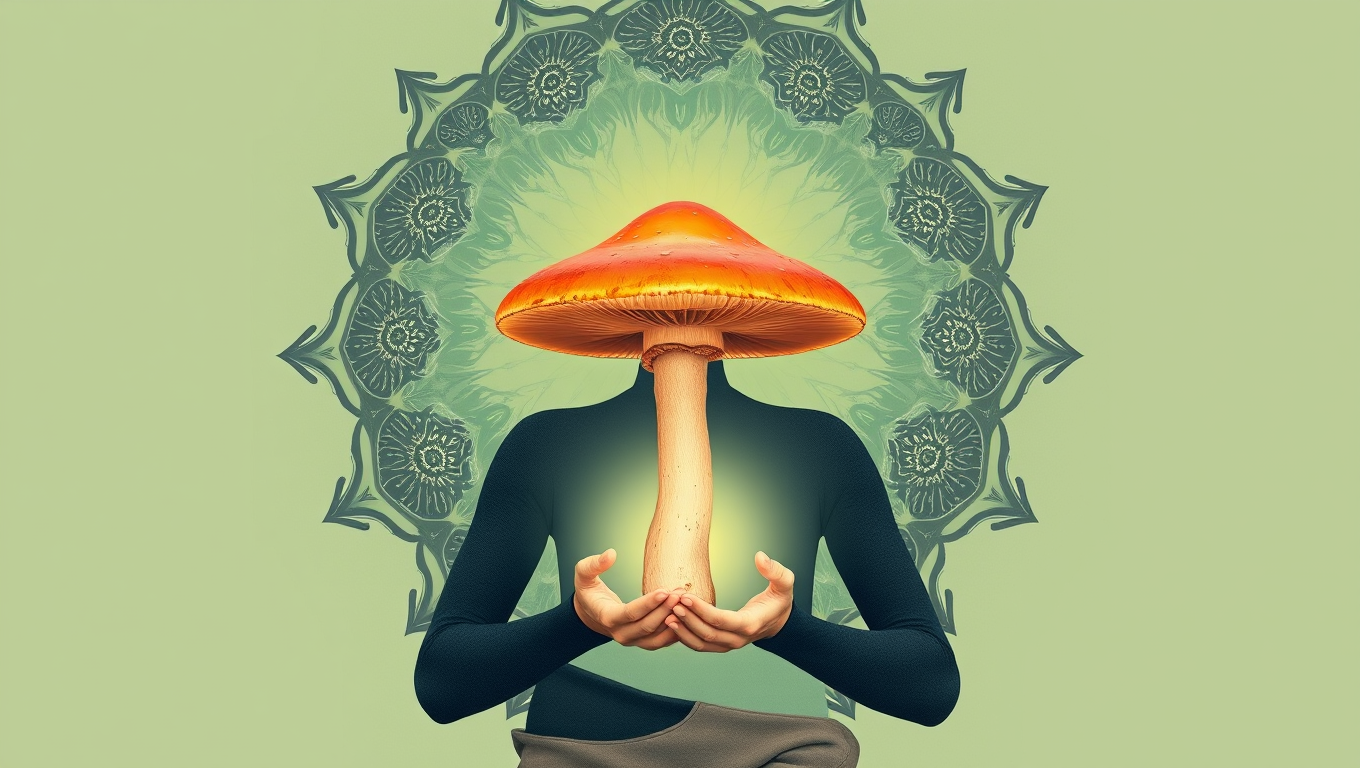
Psilocybin Use Spikes Nationwide, Especially Among Those with Mental Health Conditions
Use of psilocybin, the hallucinogenic chemical found in what is known as ‘magic mushrooms,’ has increased significantly nationwide since 2019, according to a new study.
Depression
Decoding Pain’s Dark Side: Uncovering a Hidden Brain Circuit Behind Fibromyalgia, Migraines, and PTSD
What if your brain is the reason some pain feels unbearable? Scientists at the Salk Institute have discovered a hidden brain circuit that gives pain its emotional punch—essentially transforming ordinary discomfort into lasting misery. This breakthrough sheds light on why some people suffer more intensely than others from conditions like fibromyalgia, migraines, and PTSD. By identifying the exact group of neurons that link physical pain to emotional suffering, the researchers may have found a new target for treating chronic pain—without relying on addictive medications.
Depression
The Fatigue Factor: Uncovering the Brain’s Decision-Making Process in Mental Exhaustion
When you’re mentally exhausted, your brain might be doing more behind the scenes than you think. In a new study using functional MRI, researchers uncovered two key brain regions that activate when people feel cognitively fatigued—regions that appear to weigh the cost of continuing mental effort versus giving up. Surprisingly, participants needed high financial incentives to push through challenging memory tasks, hinting that motivation can override mental fatigue. These insights may pave the way to treating brain fog in disorders like PTSD and depression using brain imaging and behavior-based therapies.
Chronic Illness
The Surprising Link Between Hearing Loss, Loneliness, and Lifespan
People who treat hearing loss with hearing aids or cochlear implants regain rich conversations, escape isolation, and may even protect their brains and lifespans—proof that better hearing translates into fuller living.
-

 Detectors3 months ago
Detectors3 months agoA New Horizon for Vision: How Gold Nanoparticles May Restore People’s Sight
-

 Earth & Climate4 months ago
Earth & Climate4 months agoRetiring Abroad Can Be Lonely Business
-

 Cancer4 months ago
Cancer4 months agoRevolutionizing Quantum Communication: Direct Connections Between Multiple Processors
-

 Agriculture and Food4 months ago
Agriculture and Food4 months ago“A Sustainable Solution: Researchers Create Hybrid Cheese with 25% Pea Protein”
-

 Diseases and Conditions4 months ago
Diseases and Conditions4 months agoReducing Falls Among Elderly Women with Polypharmacy through Exercise Intervention
-

 Albert Einstein4 months ago
Albert Einstein4 months agoHarnessing Water Waves: A Breakthrough in Controlling Floating Objects
-

 Chemistry3 months ago
Chemistry3 months ago“Unveiling Hidden Patterns: A New Twist on Interference Phenomena”
-

 Earth & Climate4 months ago
Earth & Climate4 months agoHousehold Electricity Three Times More Expensive Than Upcoming ‘Eco-Friendly’ Aviation E-Fuels, Study Reveals