While we try to keep things accurate, this content is part of an ongoing experiment and may not always be reliable.
Please double-check important details — we’re not responsible for how the information is used.
Cholesterol
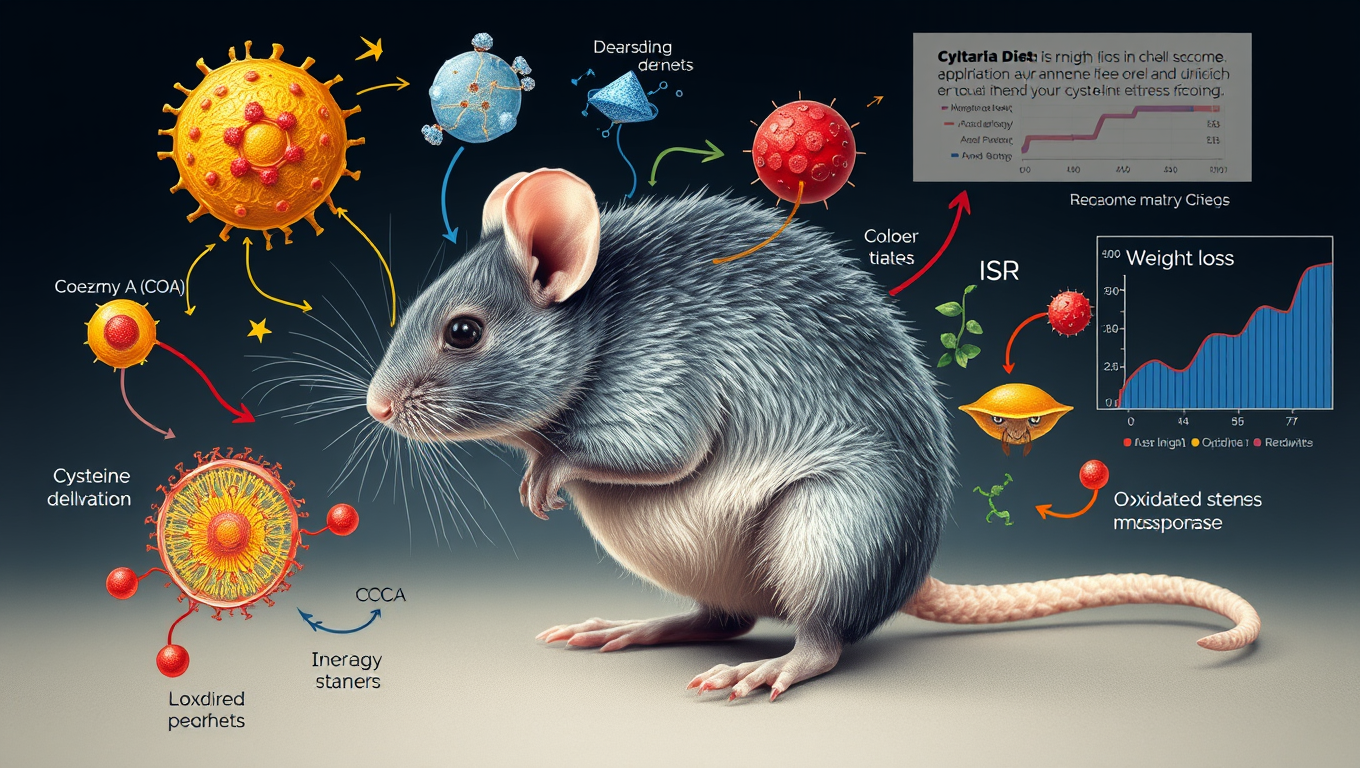
Rewiring Cellular Energy Processing for Drastic Weight Loss: A Breakthrough Mechanism
Mice genetically engineered to lack the amino acid cysteine, and fed a cysteine-free diet, lost 30 percent of their body weight in a week.
Cholesterol
Grapes Earn Superfood Status: A Scientific Case for Boosting Brain, Heart, and Gut Health
Fresh grapes contain a potent mix of over 1,600 compounds that benefit heart, brain, skin, and gut health. New evidence suggests they deserve official superfood recognition, with benefits even at the genetic level.
Cholesterol
Twice as Effective: The Surprising Benefits of Minimally Processed Foods for Weight Loss
People eating minimally processed foods lost twice as much weight as those on ultra-processed diets, even though both diets were nutritionally balanced and participants could eat freely. This real-world, long-term study revealed that food processing itself—not just nutrients—plays a significant role in shaping body weight and health outcomes.
Cholesterol
Starting Strong: Why Doctors Should Begin with High-Dose Statins to Save Lives
Potent statins are the best-proven weapon against heart disease, especially when paired with lifestyle changes. Most people aren’t active enough—and many are underdiagnosed—so starting treatment strong is key.
-

 Detectors11 months ago
Detectors11 months agoA New Horizon for Vision: How Gold Nanoparticles May Restore People’s Sight
-

 Earth & Climate12 months ago
Earth & Climate12 months agoRetiring Abroad Can Be Lonely Business
-

 Cancer12 months ago
Cancer12 months agoRevolutionizing Quantum Communication: Direct Connections Between Multiple Processors
-

 Albert Einstein12 months ago
Albert Einstein12 months agoHarnessing Water Waves: A Breakthrough in Controlling Floating Objects
-

 Chemistry11 months ago
Chemistry11 months ago“Unveiling Hidden Patterns: A New Twist on Interference Phenomena”
-

 Earth & Climate12 months ago
Earth & Climate12 months agoHousehold Electricity Three Times More Expensive Than Upcoming ‘Eco-Friendly’ Aviation E-Fuels, Study Reveals
-

 Diseases and Conditions12 months ago
Diseases and Conditions12 months agoReducing Falls Among Elderly Women with Polypharmacy through Exercise Intervention
-

 Agriculture and Food12 months ago
Agriculture and Food12 months ago“A Sustainable Solution: Researchers Create Hybrid Cheese with 25% Pea Protein”