While we try to keep things accurate, this content is part of an ongoing experiment and may not always be reliable.
Please double-check important details — we’re not responsible for how the information is used.
Breast Cancer
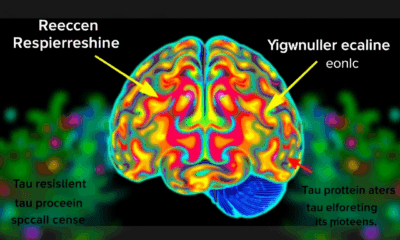
Shining a Light on Skin Cancer Risk: Misconceptions and Sociodemographic Factors
Experiencing five or more severe sunburns between the ages of 15 and 20 increases the risk of melanoma by 80% and nonmelanoma skin cancer by 68%. This study is among the few to examine the relationship between perceived cancer risk, concern about being diagnosed, confidence in health, sunburn history, and the prevalence of sun protection behaviors, all in relation to sociodemographic factors in U.S. adults. Findings reveal statistically significant associations between the number of sunburns and sociodemographic factors.

Breast Cancer
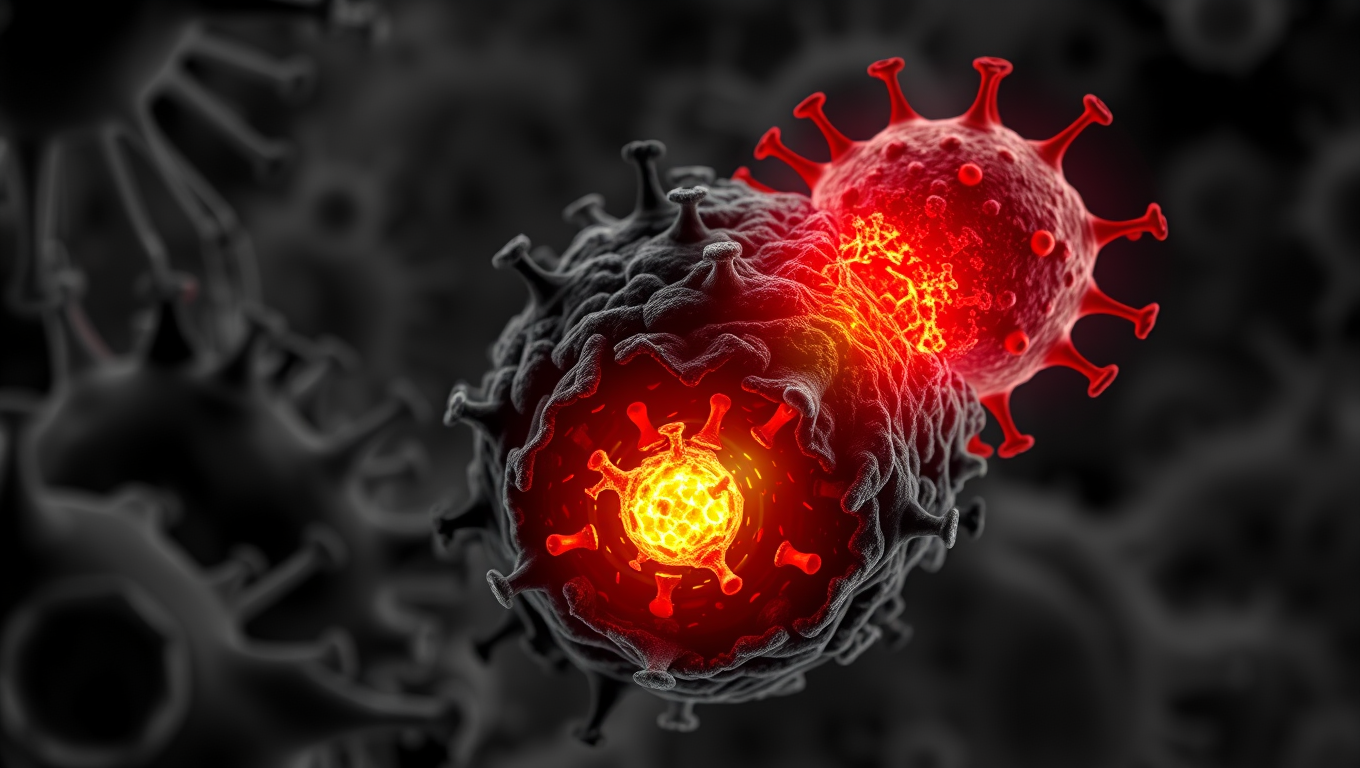
The Fatal Mutation That Lets Cancer Outsmart Our Immune System
Scientists at UC Davis discovered a small genetic difference that could explain why humans are more prone to certain cancers than our primate cousins. The change affects a protein used by immune cells to kill tumors—except in humans, it’s vulnerable to being shut down by an enzyme that tumors release. This flaw may be one reason treatments like CAR-T don’t work as well on solid tumors. The surprising twist? That mutation might have helped our brains grow larger over time. Now, researchers are exploring ways to block the enzyme and give our immune system its power back.
Anxiety
Single Psilocybin Dose Delivers Long-Term Depression Relief for Cancer Patients
Psilocybin, the active ingredient in magic mushrooms, might just revolutionize how depression and anxiety are treated in cancer patients. In a groundbreaking trial, a single dose combined with therapy significantly reduced emotional suffering, and these effects often lasted over two years. As follow-up studies expand the research to multiple doses and larger samples, scientists are eyeing a possible new standard of care that merges psychedelics with psychological support.
Brain Tumor
Groundbreaking Treatment Breakthrough: Electric Fields Supercharge Immune Assault on Brain Cancer
A breakthrough study from Keck Medicine of USC may have found a powerful new triple therapy for glioblastoma, one of the deadliest brain cancers. By combining Tumor Treating Fields (TTFields), which deliver electric waves into tumors, with immunotherapy and chemotherapy, researchers saw a major boost in survival.
-

 Detectors3 months ago
Detectors3 months agoA New Horizon for Vision: How Gold Nanoparticles May Restore People’s Sight
-

 Earth & Climate4 months ago
Earth & Climate4 months agoRetiring Abroad Can Be Lonely Business
-

 Cancer4 months ago
Cancer4 months agoRevolutionizing Quantum Communication: Direct Connections Between Multiple Processors
-

 Agriculture and Food4 months ago
Agriculture and Food4 months ago“A Sustainable Solution: Researchers Create Hybrid Cheese with 25% Pea Protein”
-

 Diseases and Conditions4 months ago
Diseases and Conditions4 months agoReducing Falls Among Elderly Women with Polypharmacy through Exercise Intervention
-

 Albert Einstein4 months ago
Albert Einstein4 months agoHarnessing Water Waves: A Breakthrough in Controlling Floating Objects
-

 Chemistry3 months ago
Chemistry3 months ago“Unveiling Hidden Patterns: A New Twist on Interference Phenomena”
-

 Earth & Climate4 months ago
Earth & Climate4 months agoHousehold Electricity Three Times More Expensive Than Upcoming ‘Eco-Friendly’ Aviation E-Fuels, Study Reveals