While we try to keep things accurate, this content is part of an ongoing experiment and may not always be reliable.
Please double-check important details — we’re not responsible for how the information is used.
Fitness
The Risks of Sedentary Behavior After a Cardiac Event
People who were less active, with a daily average of more than 14 hours of sedentary behavior, were more than twice as likely to have another cardiac event, including heart attack, surgery to treat heart issues (coronary revascularization), or to be hospitalized again within a year after the first cardiac event.

Diet and Weight Loss
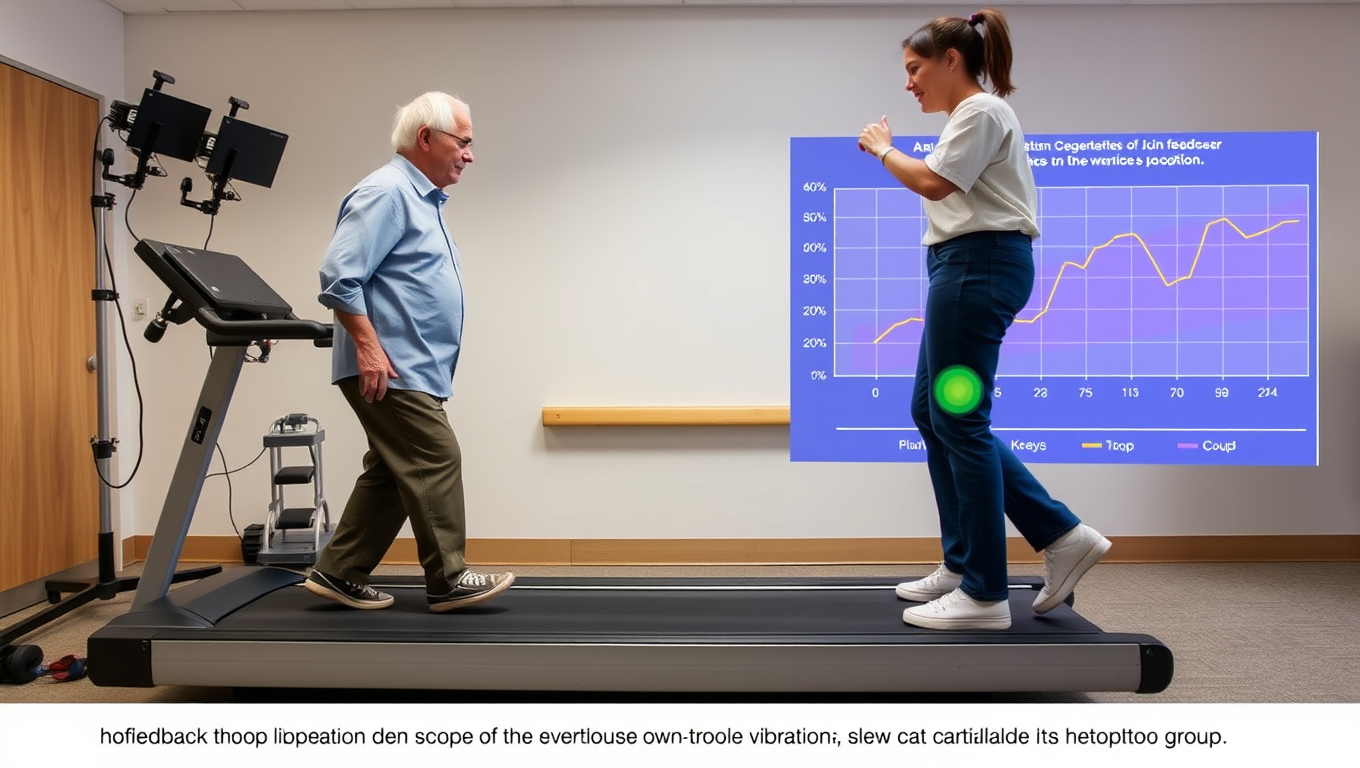
A Small Walking Adjustment Could Significantly Delay Knee Surgery for Years
A groundbreaking study has found that a simple change in walking style can ease osteoarthritis pain as effectively as medication—without the side effects. By adjusting foot angle, participants reduced knee stress, slowed cartilage damage, and maintained the change for over a year.
Alternative Medicine
A 30-Minute Workout That Could Help Slash Cancer Cell Growth
A vigorous workout can spark anti-cancer proteins, cut cancer cell growth, and help survivors fight recurrence by reducing inflammation and improving body composition.
Diabetes
Unlocking the Secret to a Calorie-Burning Furnace: Scientists Discover Key Amino Acid for Weight Loss
Cutting calories doesn’t just slim you down—it also reduces cysteine, an amino acid that flips fat cells from storage mode to fat-burning mode. Researchers found that lowering cysteine sparks the conversion of white fat into heat-producing brown fat, boosting metabolism and promoting weight loss in both humans and animal models.
-

 Detectors10 months ago
Detectors10 months agoA New Horizon for Vision: How Gold Nanoparticles May Restore People’s Sight
-

 Earth & Climate11 months ago
Earth & Climate11 months agoRetiring Abroad Can Be Lonely Business
-

 Cancer11 months ago
Cancer11 months agoRevolutionizing Quantum Communication: Direct Connections Between Multiple Processors
-

 Albert Einstein11 months ago
Albert Einstein11 months agoHarnessing Water Waves: A Breakthrough in Controlling Floating Objects
-

 Chemistry10 months ago
Chemistry10 months ago“Unveiling Hidden Patterns: A New Twist on Interference Phenomena”
-

 Earth & Climate11 months ago
Earth & Climate11 months agoHousehold Electricity Three Times More Expensive Than Upcoming ‘Eco-Friendly’ Aviation E-Fuels, Study Reveals
-

 Agriculture and Food11 months ago
Agriculture and Food11 months ago“A Sustainable Solution: Researchers Create Hybrid Cheese with 25% Pea Protein”
-

 Diseases and Conditions11 months ago
Diseases and Conditions11 months agoReducing Falls Among Elderly Women with Polypharmacy through Exercise Intervention