While we try to keep things accurate, this content is part of an ongoing experiment and may not always be reliable.
Please double-check important details — we’re not responsible for how the information is used.
Diabetes
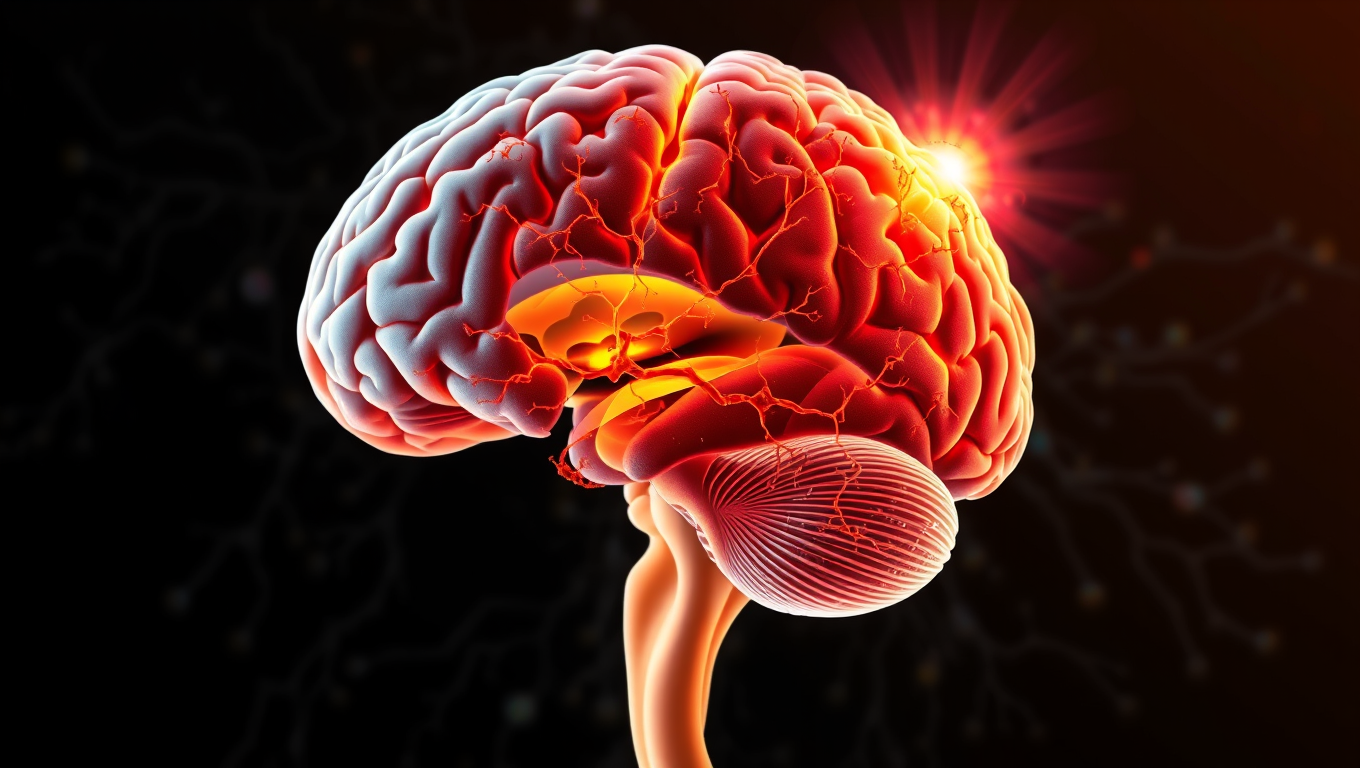
“Unraveling the Secrets of Focal Cortical Dysplasia: How Disturbed Signaling Pathways Could Promote Epileptic Seizures”
Focal cortical dysplasia (FCD) type 2 is a congenital malformation of the cerebral cortex that is often associated with difficult-to-treat epilepsy. In the affected areas, nerve cells and their layer structures are arranged in an atypical manner, which often makes drug therapy more difficult. A research team has now found evidence of profound changes in the dopamine system in FCD type 2.
Cholesterol
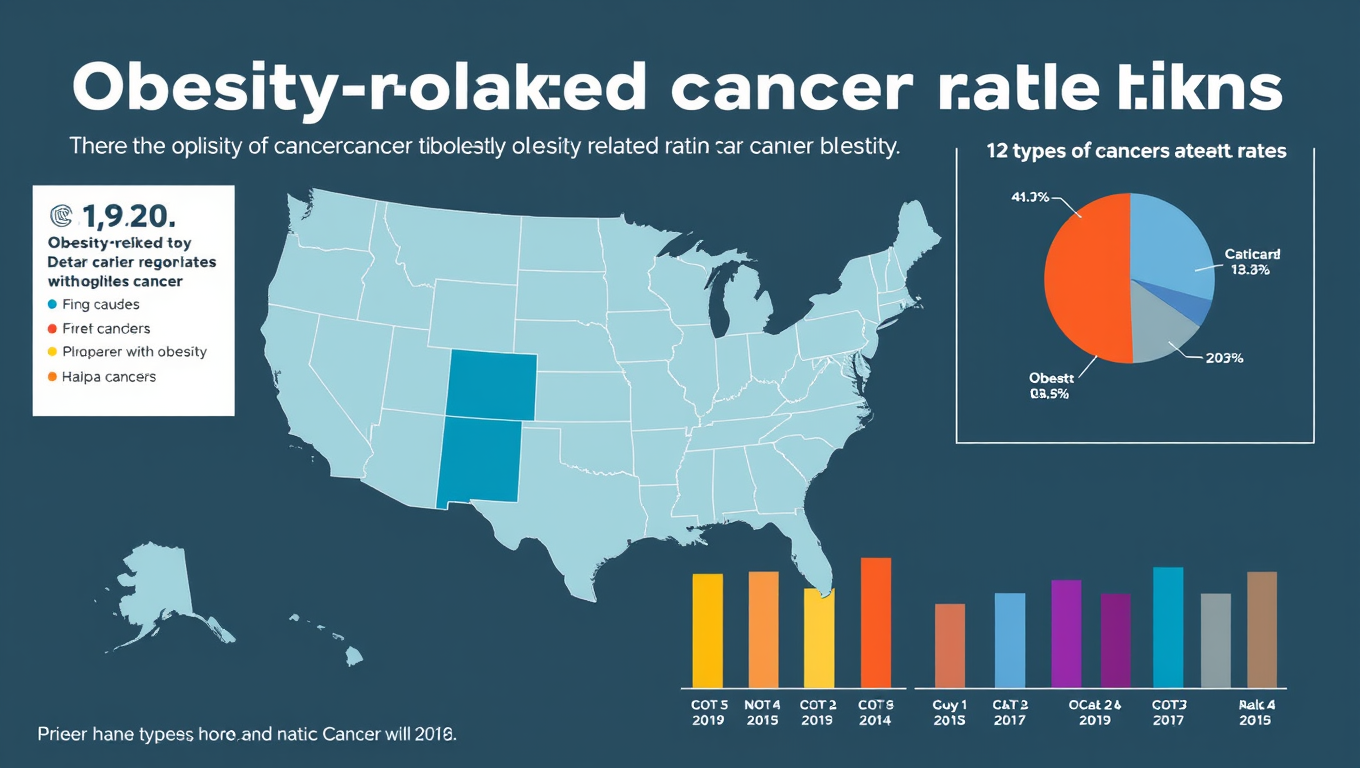
The Hidden Cancer Epidemic: How Obesity is Driving Rising Deaths Nationwide
Obesity-related cancer deaths in the U.S. have tripled in just two decades, with women, older adults, and minority groups most affected. New research presented at ENDO 2025 highlights how obesity—linked to 13 different cancers—is now a major contributor to cancer mortality, especially in underserved and rural populations. Despite the growing awareness of obesity’s broader health impacts, this surge in cancer fatalities reveals an urgent need for targeted public health interventions and equitable access to care.
Bone and Spine
The Quiet Side Effect of Semaglutide: How Losing Muscle Can Affect Weight Loss Success
Semaglutide, a popular anti-obesity drug, may come with a hidden cost: significant muscle loss, especially in women and older adults. A small study found that up to 40% of weight loss from semaglutide comes from lean body mass. Alarmingly, those who consumed less protein saw even more muscle loss—potentially undermining improvements in blood sugar control.
Diabetes
Fasting Twice a Week May Be a Game-Changer for Type 2 Diabetes Management
A new study comparing three popular diets—intermittent fasting, time-restricted eating, and continuous calorie cutting—found that all can help people with type 2 diabetes lose weight and lower blood sugar. But one diet stood out: the 5:2 intermittent fasting plan, where participants eat normally five days a week and restrict calories on two. It led to better results in fasting blood sugar, insulin response, and sticking with the plan.
-

 Detectors3 months ago
Detectors3 months agoA New Horizon for Vision: How Gold Nanoparticles May Restore People’s Sight
-

 Earth & Climate4 months ago
Earth & Climate4 months agoRetiring Abroad Can Be Lonely Business
-

 Cancer4 months ago
Cancer4 months agoRevolutionizing Quantum Communication: Direct Connections Between Multiple Processors
-

 Agriculture and Food4 months ago
Agriculture and Food4 months ago“A Sustainable Solution: Researchers Create Hybrid Cheese with 25% Pea Protein”
-

 Diseases and Conditions4 months ago
Diseases and Conditions4 months agoReducing Falls Among Elderly Women with Polypharmacy through Exercise Intervention
-

 Albert Einstein4 months ago
Albert Einstein4 months agoHarnessing Water Waves: A Breakthrough in Controlling Floating Objects
-

 Chemistry4 months ago
Chemistry4 months ago“Unveiling Hidden Patterns: A New Twist on Interference Phenomena”
-

 Earth & Climate4 months ago
Earth & Climate4 months agoHousehold Electricity Three Times More Expensive Than Upcoming ‘Eco-Friendly’ Aviation E-Fuels, Study Reveals