While we try to keep things accurate, this content is part of an ongoing experiment and may not always be reliable.
Please double-check important details — we’re not responsible for how the information is used.
Diseases and Conditions
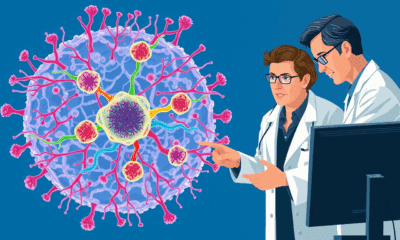
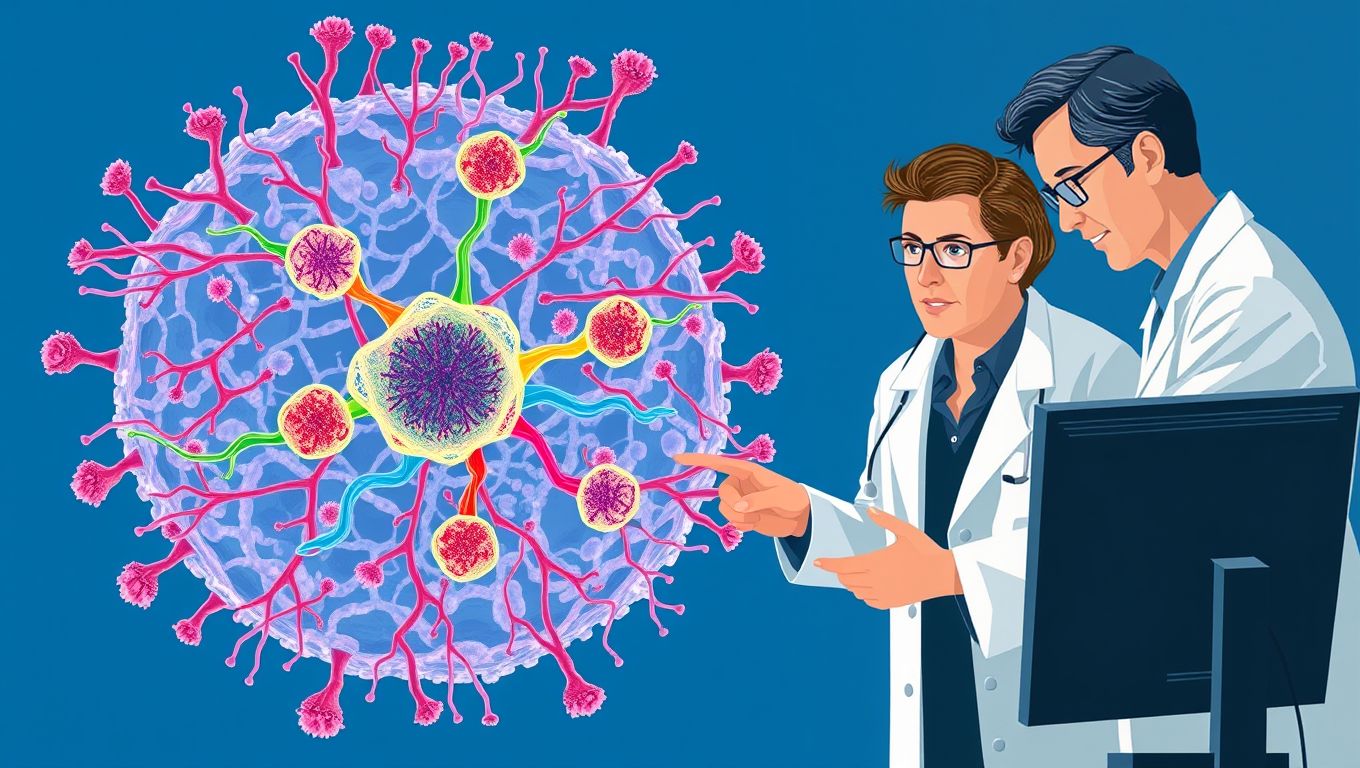
A Breakthrough Test for Lymphoma Patients: Predicting CAR T Cell Therapy Response with Machine Learning
A new article outlines a new tool that measures blood inflammation as a marker for poor CAR T therapy outcomes.

Alternative Medicine
“The Sleeping Giants: How Tai Chi, Yoga, and Jogging Rival Pills for Beating Insomnia”
Yoga, Tai Chi, walking, and jogging may be some of the best natural remedies for improving sleep and tackling insomnia, according to a large analysis comparing various treatments. While cognitive behavioral therapy (CBT) remains effective, exercise-based approaches—especially Tai Chi—were shown to deliver significant improvements in total sleep time, efficiency, and reducing how long people stay awake after falling asleep. Yoga stood out for boosting overall restfulness, and jogging helped ease insomnia symptoms.
Diseases and Conditions
Cognitive Collapse and the Nuclear Codes: When Leaders Lose Control
A shocking study reveals that many leaders of nuclear-armed nations—including US presidents and Israeli prime ministers—were afflicted by serious health problems while in office, sometimes with their conditions hidden from the public. From dementia and depression to addiction and chronic diseases, these impairments may have affected their decision-making during pivotal global crises.
Behavioral Science
“Decoding Human Tissue: Scientists Discover Five Universal Rules That Govern Organ Structure”
Scientists have uncovered a surprisingly simple “tissue code”: five rules that choreograph when, where, and how cells divide, move, and die, allowing organs like the colon to remain flawlessly organized even as they renew every few days. Mathematical models showed that manipulating just these parameters faithfully recreates real tissue architecture, hinting that the same code may govern skin, brain, and more. The discovery offers a fresh way to understand healing, birth defects, and cancer, and could supercharge initiatives such as the Human Cell Atlas by turning static cell maps into dynamic predictions.
-

 Detectors3 months ago
Detectors3 months agoA New Horizon for Vision: How Gold Nanoparticles May Restore People’s Sight
-

 Earth & Climate4 months ago
Earth & Climate4 months agoRetiring Abroad Can Be Lonely Business
-

 Cancer4 months ago
Cancer4 months agoRevolutionizing Quantum Communication: Direct Connections Between Multiple Processors
-

 Agriculture and Food4 months ago
Agriculture and Food4 months ago“A Sustainable Solution: Researchers Create Hybrid Cheese with 25% Pea Protein”
-

 Diseases and Conditions4 months ago
Diseases and Conditions4 months agoReducing Falls Among Elderly Women with Polypharmacy through Exercise Intervention
-

 Albert Einstein4 months ago
Albert Einstein4 months agoHarnessing Water Waves: A Breakthrough in Controlling Floating Objects
-

 Chemistry4 months ago
Chemistry4 months ago“Unveiling Hidden Patterns: A New Twist on Interference Phenomena”
-

 Earth & Climate4 months ago
Earth & Climate4 months agoHousehold Electricity Three Times More Expensive Than Upcoming ‘Eco-Friendly’ Aviation E-Fuels, Study Reveals