While we try to keep things accurate, this content is part of an ongoing experiment and may not always be reliable.
Please double-check important details — we’re not responsible for how the information is used.
Chronic Illness
Wildfire Smoke’s Hidden Threat: Exposure Linked to Worsening Mental Health Conditions
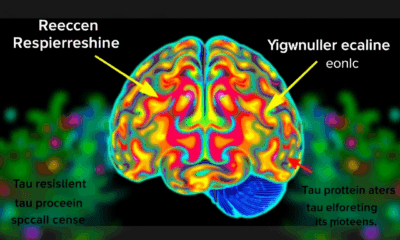
Exposure to fine particulate air pollution (PM2.5) from wildfire smoke was associated with increased visits to emergency departments (ED) for mental health conditions, according to a new study.

Animals
The Lemur Secret to Aging without Inflammation: A Breakthrough for Human Health?
What if humans didn’t have to suffer the slow-burning fire of chronic inflammation as we age? A surprising study on two types of lemurs found no evidence of “inflammaging,” a phenomenon long assumed to be universal among primates. These findings suggest that age-related inflammation isn’t inevitable and that environmental factors could play a far bigger role than we thought. By peering into the biology of our primate cousins, researchers are opening up new possibilities for preventing aging-related diseases in humans.
Chronic Illness
The Surprising Link Between Hearing Loss, Loneliness, and Lifespan
People who treat hearing loss with hearing aids or cochlear implants regain rich conversations, escape isolation, and may even protect their brains and lifespans—proof that better hearing translates into fuller living.
Alternative Medicine
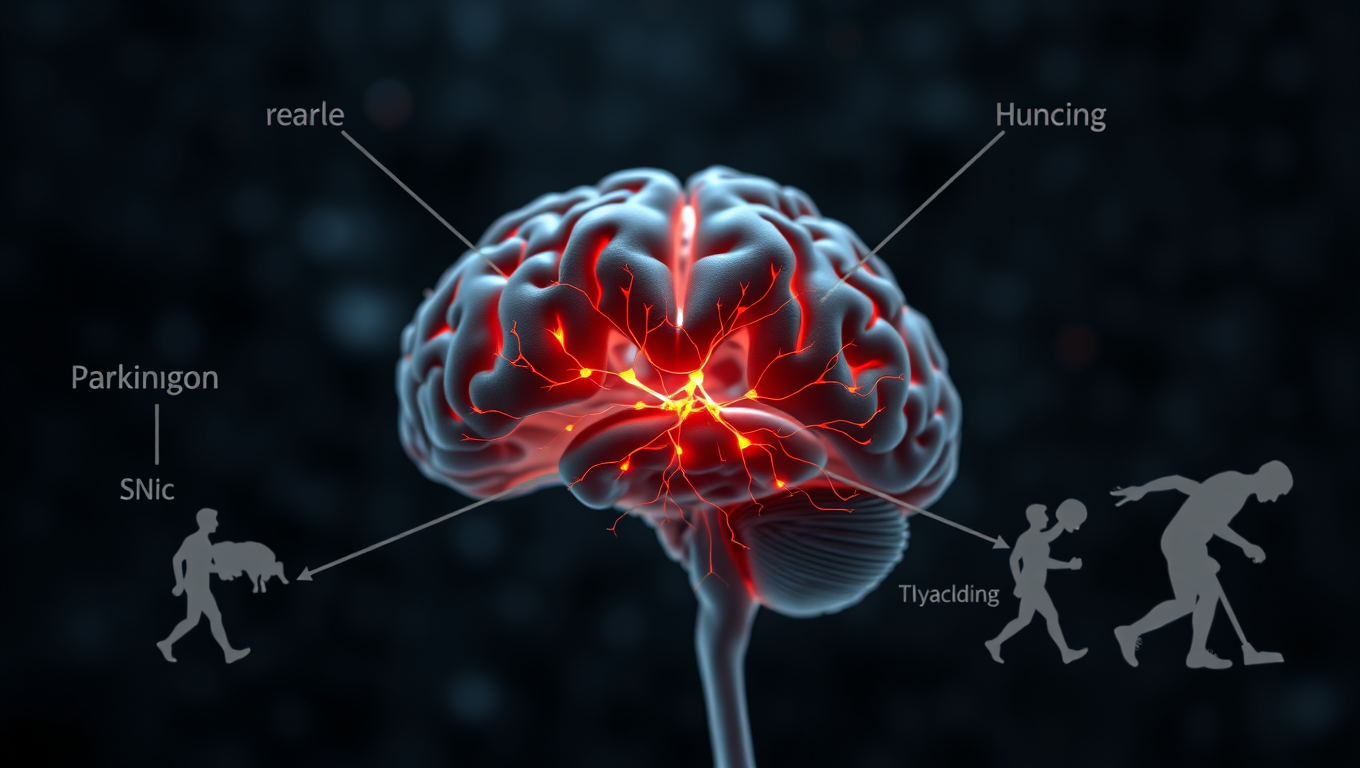
Catching Parkinson’s Sooner: Tiny Twitches, Big Breakthroughs
These findings highlight the significance of rearing behavior and behavioral lateralization as potential behavioral markers for tracking the progression of Parkinson's disease.
-

 Detectors3 months ago
Detectors3 months agoA New Horizon for Vision: How Gold Nanoparticles May Restore People’s Sight
-

 Earth & Climate4 months ago
Earth & Climate4 months agoRetiring Abroad Can Be Lonely Business
-

 Cancer4 months ago
Cancer4 months agoRevolutionizing Quantum Communication: Direct Connections Between Multiple Processors
-

 Agriculture and Food4 months ago
Agriculture and Food4 months ago“A Sustainable Solution: Researchers Create Hybrid Cheese with 25% Pea Protein”
-

 Diseases and Conditions4 months ago
Diseases and Conditions4 months agoReducing Falls Among Elderly Women with Polypharmacy through Exercise Intervention
-

 Albert Einstein4 months ago
Albert Einstein4 months agoHarnessing Water Waves: A Breakthrough in Controlling Floating Objects
-

 Chemistry4 months ago
Chemistry4 months ago“Unveiling Hidden Patterns: A New Twist on Interference Phenomena”
-

 Earth & Climate4 months ago
Earth & Climate4 months agoHousehold Electricity Three Times More Expensive Than Upcoming ‘Eco-Friendly’ Aviation E-Fuels, Study Reveals