While we try to keep things accurate, this content is part of an ongoing experiment and may not always be reliable.
Please double-check important details — we’re not responsible for how the information is used.
Cystic Fibrosis
A New Path to Early Diagnosis: Recommendations for Improving Cystic Fibrosis Screening in Infants
The United States Cystic Fibrosis Foundation released the first guideline on newborn screening for cystic fibrosis (CF), in order to improve timely detection of CF in infants from all racial and ethnic backgrounds. The new guideline reflects rigorous scientific investigation and perspectives from parents, CF specialists, public health representatives, primary care providers and genetic counselors.

COPD
Revolutionary Nanoparticles Deliver Genetic Treatments Directly to the Lungs
A scientific team has unlocked a new way to treat serious lung conditions by using specially designed nanoparticles to deliver genetic therapies straight to lung cells. This innovation could transform care for patients with cystic fibrosis or lung cancer. With a powerful combination of gene editing and RNA delivery, the system has already shown promise in animal trials. The streamlined approach not only enhances precision but also avoids harmful side effects, making it a bold leap forward in respiratory medicine.
Chronic Illness
Diabetes Pill Shows Promise in Reducing Liver Scarring
A diabetes drug may soon double as a treatment for liver disease. Dapagliflozin, an SGLT-2 inhibitor typically used for type 2 diabetes, significantly improved liver inflammation and scarring in patients with metabolic dysfunction-associated steatohepatitis (MASH) during a clinical trial in China. Participants on the drug saw better liver outcomes and fewer side effects than those on a placebo. Although more research is needed, especially in diverse populations, this finding hints at a transformative role for existing medications in tackling liver diseases.
Biology
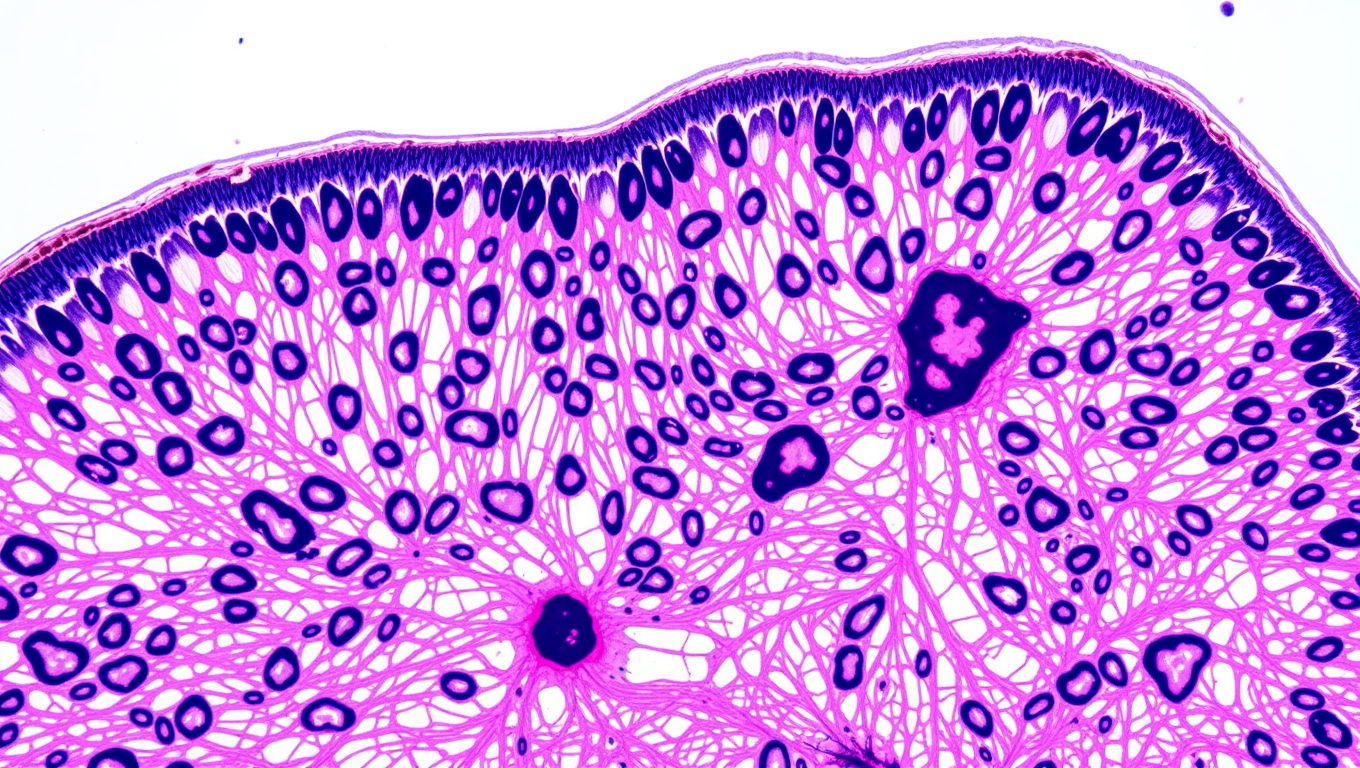
Yeast Revolutionizes Human Protein Production with DNase1 Breakthrough
The protein DNase1 is one of the oldest biological agents in history: It has been on the market since 1958 and is now used, among other things, to treat cystic fibrosis. However, it takes considerable effort to produce it in immortalized hamster cells. This process is also costly. It would be far more cost-effective to produce it with undemanding yeast cells.
-

 Detectors11 months ago
Detectors11 months agoA New Horizon for Vision: How Gold Nanoparticles May Restore People’s Sight
-

 Cancer12 months ago
Cancer12 months agoRevolutionizing Quantum Communication: Direct Connections Between Multiple Processors
-

 Earth & Climate12 months ago
Earth & Climate12 months agoRetiring Abroad Can Be Lonely Business
-

 Albert Einstein12 months ago
Albert Einstein12 months agoHarnessing Water Waves: A Breakthrough in Controlling Floating Objects
-

 Chemistry11 months ago
Chemistry11 months ago“Unveiling Hidden Patterns: A New Twist on Interference Phenomena”
-

 Earth & Climate11 months ago
Earth & Climate11 months agoHousehold Electricity Three Times More Expensive Than Upcoming ‘Eco-Friendly’ Aviation E-Fuels, Study Reveals
-

 Agriculture and Food12 months ago
Agriculture and Food12 months ago“A Sustainable Solution: Researchers Create Hybrid Cheese with 25% Pea Protein”
-

 Diseases and Conditions12 months ago
Diseases and Conditions12 months agoReducing Falls Among Elderly Women with Polypharmacy through Exercise Intervention