While we try to keep things accurate, this content is part of an ongoing experiment and may not always be reliable.
Please double-check important details — we’re not responsible for how the information is used.
Alzheimer's
Diagnostic Uncertainty in Parkinson’s Disease: A Study Highlights Need for Improved Diagnostic Processes
A study found that a significant proportion of Parkinson’s disease diagnoses are later corrected. Up to one in six diagnoses changed after ten years of follow-up, and the majority of new diagnoses were made within two years of the original diagnosis.

Alzheimer's
Unlocking the Brain’s Sugar Code: Scientists Discover a New Player in the Battle Against Alzheimer’s
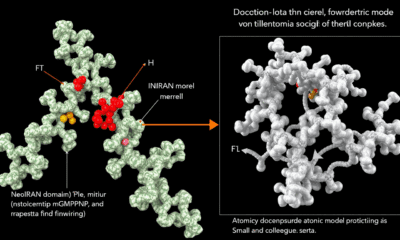
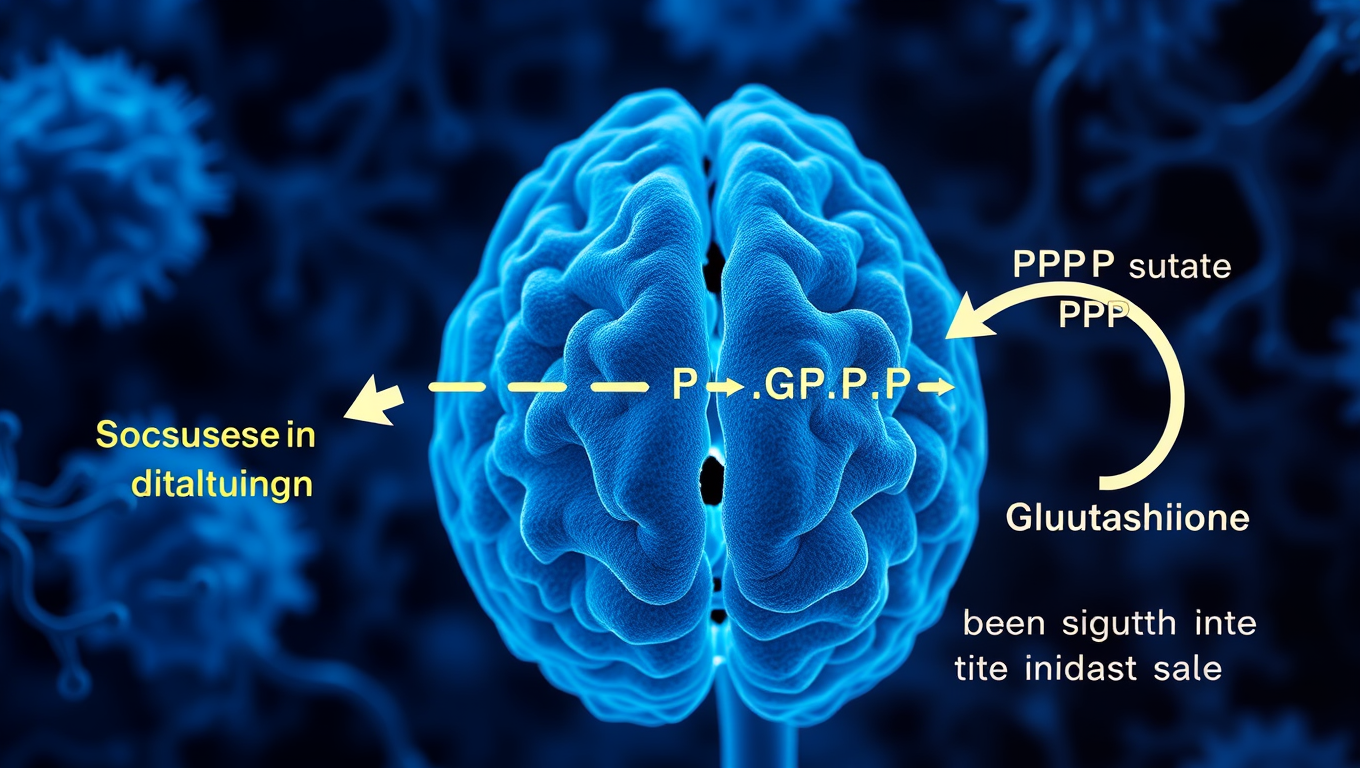
Scientists have uncovered a surprising sugar-related mechanism inside brain cells that could transform how we fight Alzheimer’s and other dementias. It turns out neurons don’t just store sugar for fuel—they reroute it to power antioxidant defenses, but only if an enzyme called GlyP is active. When this sugar-clearing system is blocked, toxic tau protein builds up and accelerates brain degeneration.
Alzheimer's
Groundbreaking Study Suggests Link Between Semaglutide and Lower Dementia Risk in Type 2 Diabetes Patients
A blockbuster diabetes and weight-loss drug might be doing more than controlling blood sugar—it could also be protecting the brain. Researchers at Case Western Reserve University found that people with type 2 diabetes who took semaglutide (the active ingredient in Ozempic and Wegovy) had a significantly lower risk of developing dementia. The benefit was especially strong in women and older adults.
Alzheimer's
The Common Blood Test That Could Predict Alzheimer’s Progression
A simple blood test could reveal which early Alzheimer’s patients are most at risk for rapid decline. Researchers found that people with high insulin resistance—measured by the TyG index—were four times more likely to experience faster cognitive deterioration. The study highlights a major opportunity: a common lab value already available in hospitals could help guide personalized treatment strategies. This discovery also uncovers a unique vulnerability in Alzheimer’s disease to metabolic stress, offering new possibilities for intervention while the disease is still in its early stages.
-

 Detectors3 months ago
Detectors3 months agoA New Horizon for Vision: How Gold Nanoparticles May Restore People’s Sight
-

 Earth & Climate4 months ago
Earth & Climate4 months agoRetiring Abroad Can Be Lonely Business
-

 Cancer4 months ago
Cancer4 months agoRevolutionizing Quantum Communication: Direct Connections Between Multiple Processors
-

 Agriculture and Food4 months ago
Agriculture and Food4 months ago“A Sustainable Solution: Researchers Create Hybrid Cheese with 25% Pea Protein”
-

 Diseases and Conditions4 months ago
Diseases and Conditions4 months agoReducing Falls Among Elderly Women with Polypharmacy through Exercise Intervention
-

 Albert Einstein4 months ago
Albert Einstein4 months agoHarnessing Water Waves: A Breakthrough in Controlling Floating Objects
-

 Chemistry3 months ago
Chemistry3 months ago“Unveiling Hidden Patterns: A New Twist on Interference Phenomena”
-

 Earth & Climate3 months ago
Earth & Climate3 months agoHousehold Electricity Three Times More Expensive Than Upcoming ‘Eco-Friendly’ Aviation E-Fuels, Study Reveals