While we try to keep things accurate, this content is part of an ongoing experiment and may not always be reliable.
Please double-check important details — we’re not responsible for how the information is used.
Cholesterol
The Dark Side of Diet: How High-Fat, High-Sugar Diets Affect Brain Function
New research links fatty, sugary diets to impaired brain function. The findings build on a growing body of evidence showing the negative impact of high-fat, high-sugar (HFHS) diets on cognitive ability, adding to their well-known physical effects.

Cholesterol
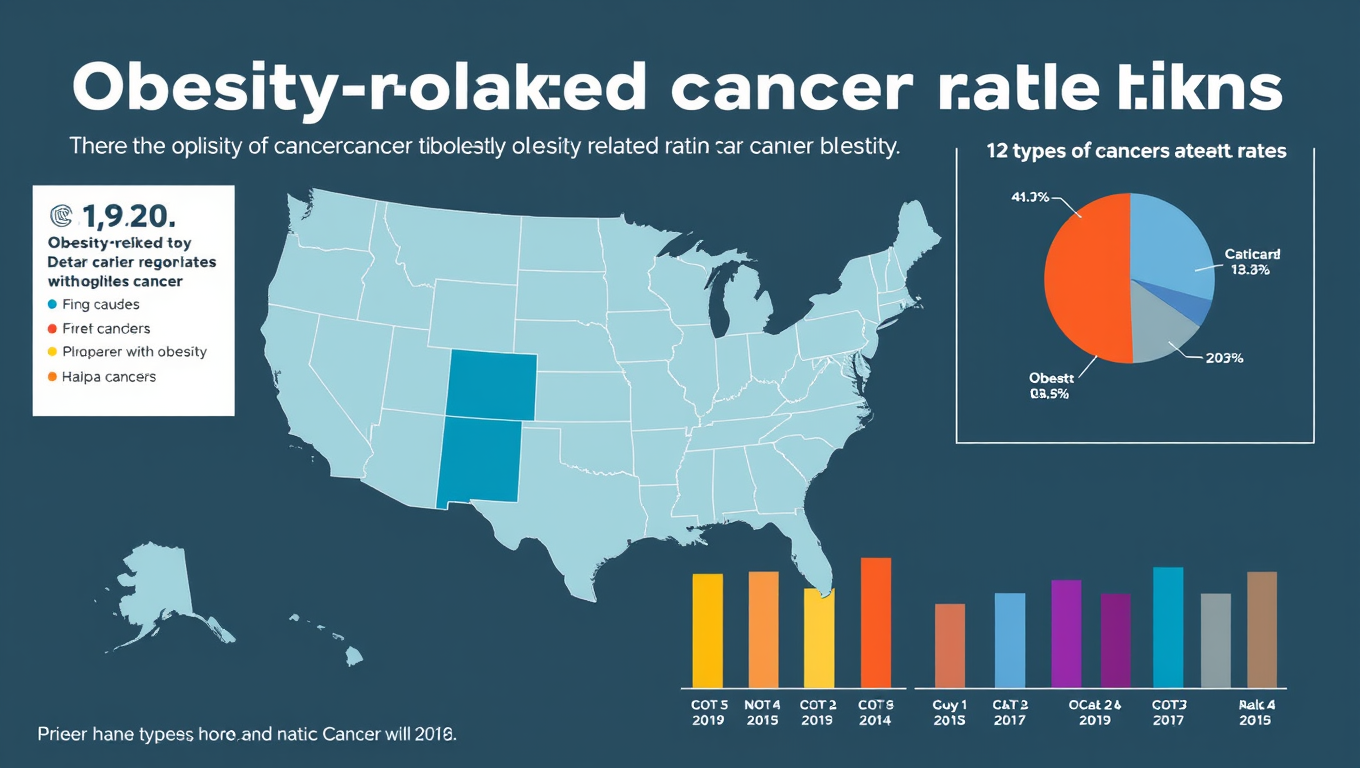
The Hidden Cancer Epidemic: How Obesity is Driving Rising Deaths Nationwide
Obesity-related cancer deaths in the U.S. have tripled in just two decades, with women, older adults, and minority groups most affected. New research presented at ENDO 2025 highlights how obesity—linked to 13 different cancers—is now a major contributor to cancer mortality, especially in underserved and rural populations. Despite the growing awareness of obesity’s broader health impacts, this surge in cancer fatalities reveals an urgent need for targeted public health interventions and equitable access to care.
Cholesterol
The Dark Side of Healthy Fats: How Oleic Acid May Be Fueling Obesity
A popular fat found in olive oil may not be as innocent as it seems. Scientists discovered that oleic acid, a major component of many high-fat foods, uniquely spurs the growth of new fat cells by manipulating specific proteins in the body. Unlike other fats, it boosts the number of “fat cell soldiers,” setting the stage for obesity and possibly chronic diseases. This unexpected twist reveals that the type of fat we eat, not just how much, may play a crucial role in our health.
Anemia
Hidden Risk: Three Genetic Variants That Raise Clot Risk by 180%
Genetic research in Sweden has unveiled three new gene variants that dramatically increase the risk of venous blood clots, sometimes by up to 180%. These discoveries build on existing knowledge of Factor V Leiden and suggest that genetics plays a bigger role than previously thought, especially for clots in the legs that can lead to life-threatening pulmonary embolisms.
-

 Detectors3 months ago
Detectors3 months agoA New Horizon for Vision: How Gold Nanoparticles May Restore People’s Sight
-

 Earth & Climate4 months ago
Earth & Climate4 months agoRetiring Abroad Can Be Lonely Business
-

 Cancer4 months ago
Cancer4 months agoRevolutionizing Quantum Communication: Direct Connections Between Multiple Processors
-

 Agriculture and Food4 months ago
Agriculture and Food4 months ago“A Sustainable Solution: Researchers Create Hybrid Cheese with 25% Pea Protein”
-

 Diseases and Conditions4 months ago
Diseases and Conditions4 months agoReducing Falls Among Elderly Women with Polypharmacy through Exercise Intervention
-

 Chemistry4 months ago
Chemistry4 months ago“Unveiling Hidden Patterns: A New Twist on Interference Phenomena”
-

 Albert Einstein4 months ago
Albert Einstein4 months agoHarnessing Water Waves: A Breakthrough in Controlling Floating Objects
-

 Earth & Climate4 months ago
Earth & Climate4 months agoHousehold Electricity Three Times More Expensive Than Upcoming ‘Eco-Friendly’ Aviation E-Fuels, Study Reveals