While we try to keep things accurate, this content is part of an ongoing experiment and may not always be reliable.
Please double-check important details — we’re not responsible for how the information is used.
Dementia
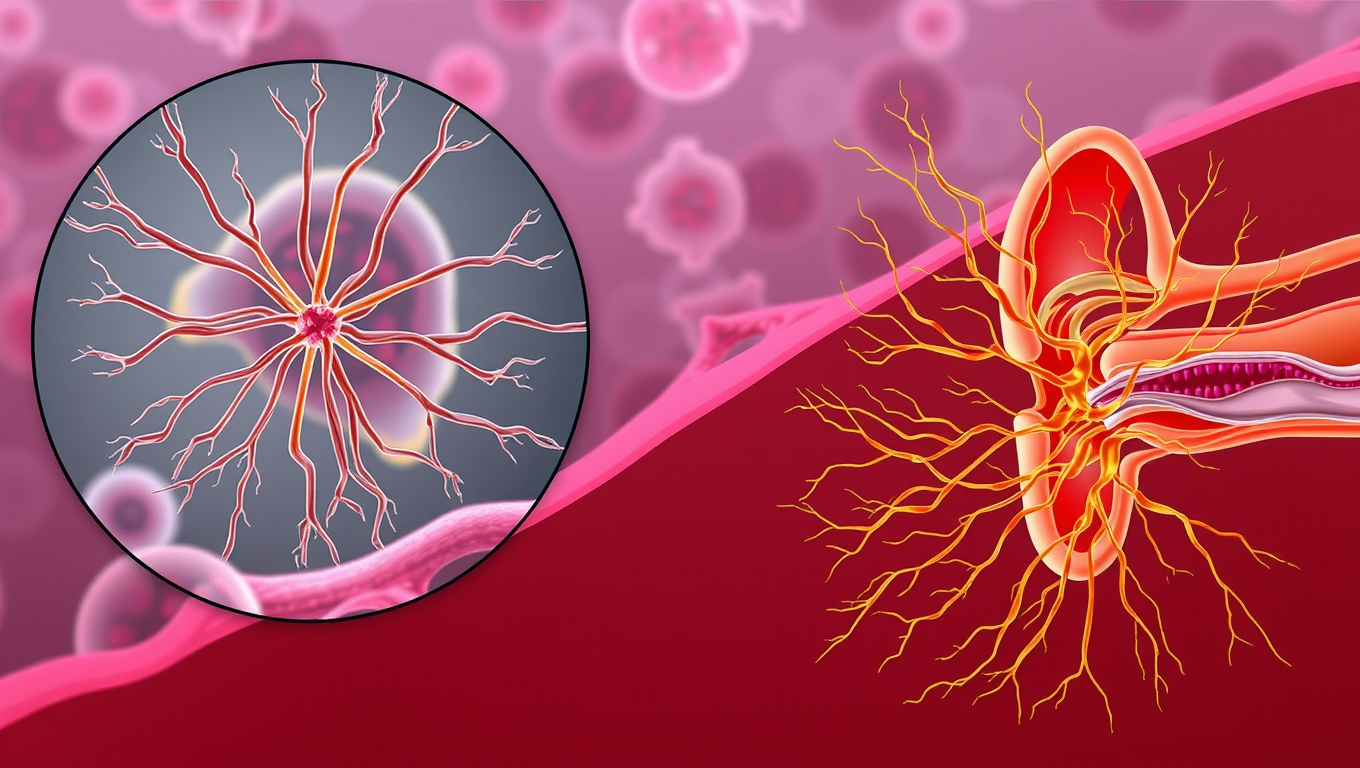
The Fine Control of Cell Mechanics Unveiled
Our skin and mucous membranes are protected by epithelial cells. This ‘barrier’ tissue performs its function thanks to specialized structures called ‘junctions’. They ensure cell cohesion and regulate exchanges across the space between cells. Researchers have studied the role of a specific protein, gamma-actin, in the organization and mechanics of epithelial cells and their junctions. Their work reveals a mechanism of interdependence of different forms of the cytoskeletal proteins actin and myosin, and their functions. The team also demonstrates the key role of gamma-actin in the rigidity of cell membranes and the dynamics of junctional proteins, which may provide a mechanism of hearing loss.
Dementia
Unlocking the Secrets of Women’s Alzheimer’s Risk: Omega-3 Deficiency Revealed
Researchers discovered that women with Alzheimer’s show a sharp loss of omega fatty acids, unlike men, pointing to sex-specific differences in the disease. The study suggests omega-rich diets could be key, but clinical trials are needed.
Dementia
Unraveling Brain Aging: The Breakthrough Discovery of FTL1 Protein
Scientists at UCSF have uncovered a surprising culprit behind brain aging: a protein called FTL1. In mice, too much FTL1 caused memory loss, weaker brain connections, and sluggish cells. But when researchers blocked it, the animals regained youthful brain function and sharp memory. The discovery suggests that one protein could be the master switch for aging in the brain — and targeting it may one day allow us to actually reverse cognitive decline, not just slow it down.
Alzheimer's
Scientists Unlock Secret to Reversing Memory Loss by Boosting Brain’s Energy Engines
Scientists have discovered a direct cause-and-effect link between faulty mitochondria and the memory loss seen in neurodegenerative diseases. By creating a novel tool to boost mitochondrial activity in mouse models, researchers restored memory performance, suggesting mitochondria could be a powerful new target for treatments. The findings not only shed light on the early drivers of brain cell degeneration but also open possibilities for slowing or even preventing diseases like Alzheimer’s.
-

 Detectors10 months ago
Detectors10 months agoA New Horizon for Vision: How Gold Nanoparticles May Restore People’s Sight
-

 Earth & Climate11 months ago
Earth & Climate11 months agoRetiring Abroad Can Be Lonely Business
-

 Cancer11 months ago
Cancer11 months agoRevolutionizing Quantum Communication: Direct Connections Between Multiple Processors
-

 Albert Einstein11 months ago
Albert Einstein11 months agoHarnessing Water Waves: A Breakthrough in Controlling Floating Objects
-

 Chemistry11 months ago
Chemistry11 months ago“Unveiling Hidden Patterns: A New Twist on Interference Phenomena”
-

 Earth & Climate11 months ago
Earth & Climate11 months agoHousehold Electricity Three Times More Expensive Than Upcoming ‘Eco-Friendly’ Aviation E-Fuels, Study Reveals
-

 Agriculture and Food11 months ago
Agriculture and Food11 months ago“A Sustainable Solution: Researchers Create Hybrid Cheese with 25% Pea Protein”
-

 Diseases and Conditions11 months ago
Diseases and Conditions11 months agoReducing Falls Among Elderly Women with Polypharmacy through Exercise Intervention