While we try to keep things accurate, this content is part of an ongoing experiment and may not always be reliable.
Please double-check important details — we’re not responsible for how the information is used.
Alzheimer's Research
Unlocking New Therapies: Largest Osteoarthritis Genetic Study Reveals Pathways to Treatment Advancements
Researchers have uncovered multiple new genes and genetic pathways that could lead to repurposing hundreds of existing drugs for osteoarthritis, the most common form of arthritis.

Alternative Medicine
A Pain-Free Patch Revolutionizes Cancer Detection with Nanoneedles
A new nanotechnology breakthrough may soon eliminate the need for painful biopsies. Scientists have developed a patch filled with nanoneedles thinner than a human hair that can painlessly extract molecular data from tissues without removing or damaging them. This enables real-time disease monitoring, particularly for conditions like brain cancer and Alzheimer s, and could radically change how doctors diagnose and track disease. The patch works quickly, integrates with common medical tools, and provides results using AI, opening doors to personalized medicine and better surgical decisions.
Alzheimer's
Epilepsy Strikes with Surprising Frequency in Frontotemporal Dementia Patients
According to a recent study, in patients with frontotemporal dementia (FTD), epileptic seizures are significantly more common than previously known. The discovery deepens understanding of the symptoms of this memory disorder and emphasises the importance of taking epileptic seizures into account in the treatment and monitoring of patients.
Alzheimer's
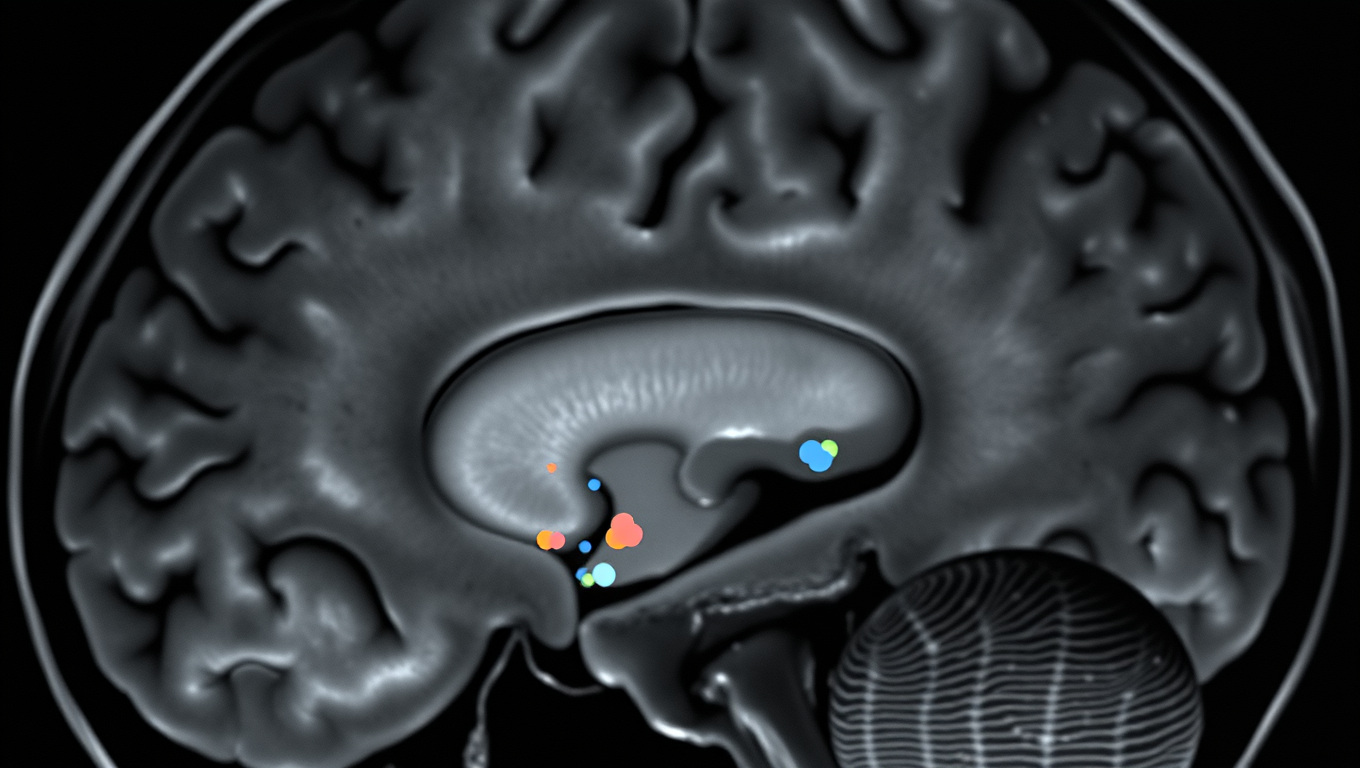
Breaking New Ground: Immune System Discovery Offers Potential Solution to Alzheimer’s
A new way of thinking about Alzheimer’s disease has yielded a discovery that could be the key to stopping the cognitive decline seen in Alzheimer’s and other neurodegenerative diseases, including ALS and Parkinson’s.
-

 Detectors3 months ago
Detectors3 months agoA New Horizon for Vision: How Gold Nanoparticles May Restore People’s Sight
-

 Earth & Climate4 months ago
Earth & Climate4 months agoRetiring Abroad Can Be Lonely Business
-

 Cancer3 months ago
Cancer3 months agoRevolutionizing Quantum Communication: Direct Connections Between Multiple Processors
-

 Agriculture and Food4 months ago
Agriculture and Food4 months ago“A Sustainable Solution: Researchers Create Hybrid Cheese with 25% Pea Protein”
-

 Diseases and Conditions4 months ago
Diseases and Conditions4 months agoReducing Falls Among Elderly Women with Polypharmacy through Exercise Intervention
-

 Chemistry3 months ago
Chemistry3 months ago“Unveiling Hidden Patterns: A New Twist on Interference Phenomena”
-

 Albert Einstein4 months ago
Albert Einstein4 months agoHarnessing Water Waves: A Breakthrough in Controlling Floating Objects
-

 Earth & Climate3 months ago
Earth & Climate3 months agoHousehold Electricity Three Times More Expensive Than Upcoming ‘Eco-Friendly’ Aviation E-Fuels, Study Reveals