While we try to keep things accurate, this content is part of an ongoing experiment and may not always be reliable.
Please double-check important details — we’re not responsible for how the information is used.
Diseases and Conditions
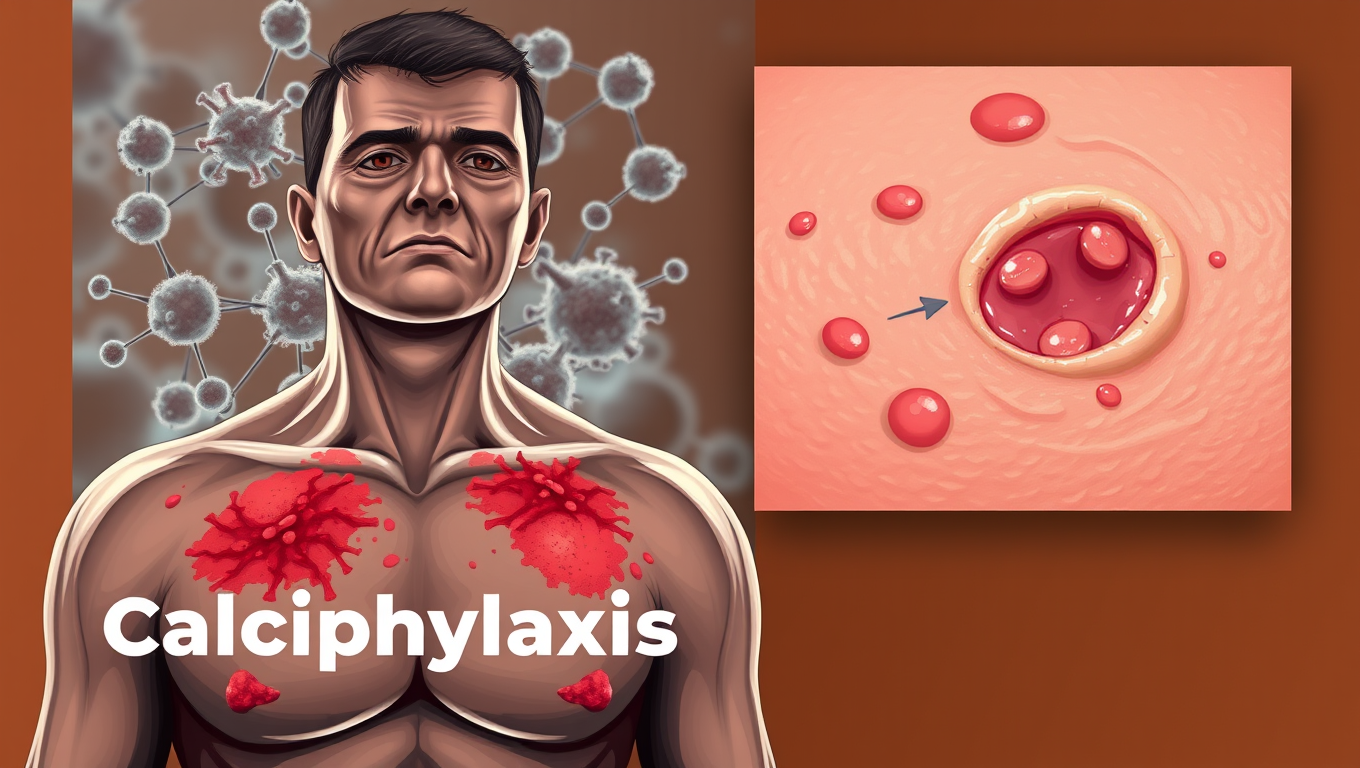
Unlocking the Mystery of Calciphylaxis: Researchers Identify Key Pathway Responsible for Rare and Serious Condition
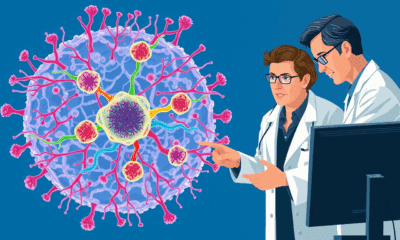
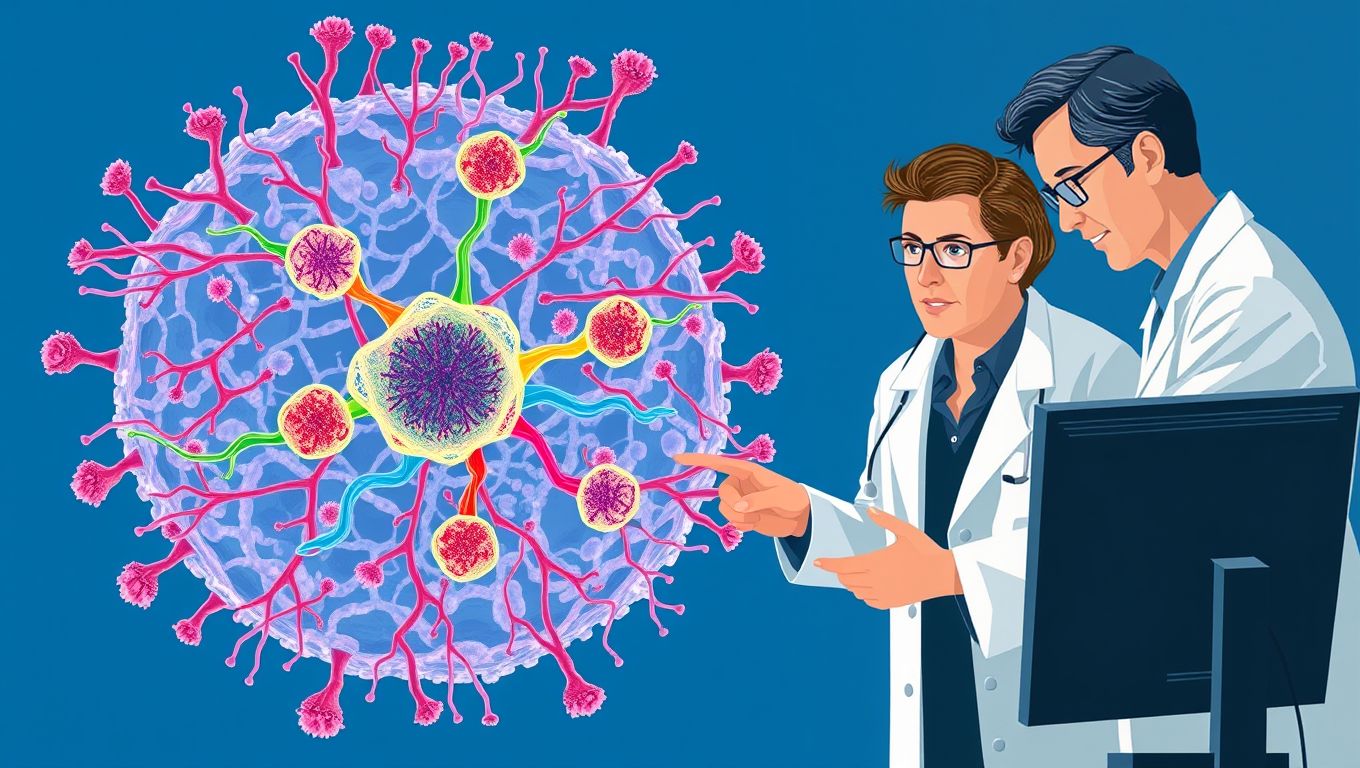
The global burden of chronic kidney disease (CKD) is rising, with more than 800 million people affected worldwide. Vascular diseases in patients with CKD are unique and grouped as uremic vascular diseases. One of them, calciphylaxis, typically affects patients with end-stage, advanced kidney disease. It is a condition characterized by severe, painful and non-healing skin ulcers with no known cure. Researchers have now discovered a novel biological pathway, called the IL6 pathway, central to the skin lesion initiation and progression. Blocking this pathway they believe, will likely prevent progression of the skin ulcers and resolve the pain seen in patients with calciphylaxis.
Diseases and Conditions
Cognitive Collapse and the Nuclear Codes: When Leaders Lose Control
A shocking study reveals that many leaders of nuclear-armed nations—including US presidents and Israeli prime ministers—were afflicted by serious health problems while in office, sometimes with their conditions hidden from the public. From dementia and depression to addiction and chronic diseases, these impairments may have affected their decision-making during pivotal global crises.
Behavioral Science
“Decoding Human Tissue: Scientists Discover Five Universal Rules That Govern Organ Structure”
Scientists have uncovered a surprisingly simple “tissue code”: five rules that choreograph when, where, and how cells divide, move, and die, allowing organs like the colon to remain flawlessly organized even as they renew every few days. Mathematical models showed that manipulating just these parameters faithfully recreates real tissue architecture, hinting that the same code may govern skin, brain, and more. The discovery offers a fresh way to understand healing, birth defects, and cancer, and could supercharge initiatives such as the Human Cell Atlas by turning static cell maps into dynamic predictions.
ADD and ADHD
Breaking the Cycle: How ADHD and Insomnia Can Intersect to Affect Quality of Life
Struggling to sleep might be the hidden reason why adults with ADHD traits often feel less satisfied with life. New research reveals a strong link between insomnia and reduced well-being in people with ADHD symptoms, suggesting a vicious cycle where poor sleep worsens attention and emotional issues, and vice versa.
-

 Detectors3 months ago
Detectors3 months agoA New Horizon for Vision: How Gold Nanoparticles May Restore People’s Sight
-

 Earth & Climate4 months ago
Earth & Climate4 months agoRetiring Abroad Can Be Lonely Business
-

 Cancer4 months ago
Cancer4 months agoRevolutionizing Quantum Communication: Direct Connections Between Multiple Processors
-

 Agriculture and Food4 months ago
Agriculture and Food4 months ago“A Sustainable Solution: Researchers Create Hybrid Cheese with 25% Pea Protein”
-

 Albert Einstein4 months ago
Albert Einstein4 months agoHarnessing Water Waves: A Breakthrough in Controlling Floating Objects
-

 Diseases and Conditions4 months ago
Diseases and Conditions4 months agoReducing Falls Among Elderly Women with Polypharmacy through Exercise Intervention
-

 Chemistry4 months ago
Chemistry4 months ago“Unveiling Hidden Patterns: A New Twist on Interference Phenomena”
-

 Earth & Climate4 months ago
Earth & Climate4 months agoHousehold Electricity Three Times More Expensive Than Upcoming ‘Eco-Friendly’ Aviation E-Fuels, Study Reveals