While we try to keep things accurate, this content is part of an ongoing experiment and may not always be reliable.
Please double-check important details — we’re not responsible for how the information is used.
Caregiving
“Collaborative Care: How Nurses and AI are Working Together to Save Lives and Reduce Hospital Stays”
An AI tool that analyzes nurses’ data and notes detected when patients in the hospital were deteriorating nearly two days earlier than traditional methods and reduced the risk of death by over 35%.

Brain Injury
Brain Training Game Offers New Hope for Drug-Free Pain Management
A trial of an interactive game that trains people to alter their brain waves has shown promise as a treatment for nerve pain — offering hope for a new generation of drug-free treatments.
Alzheimer's
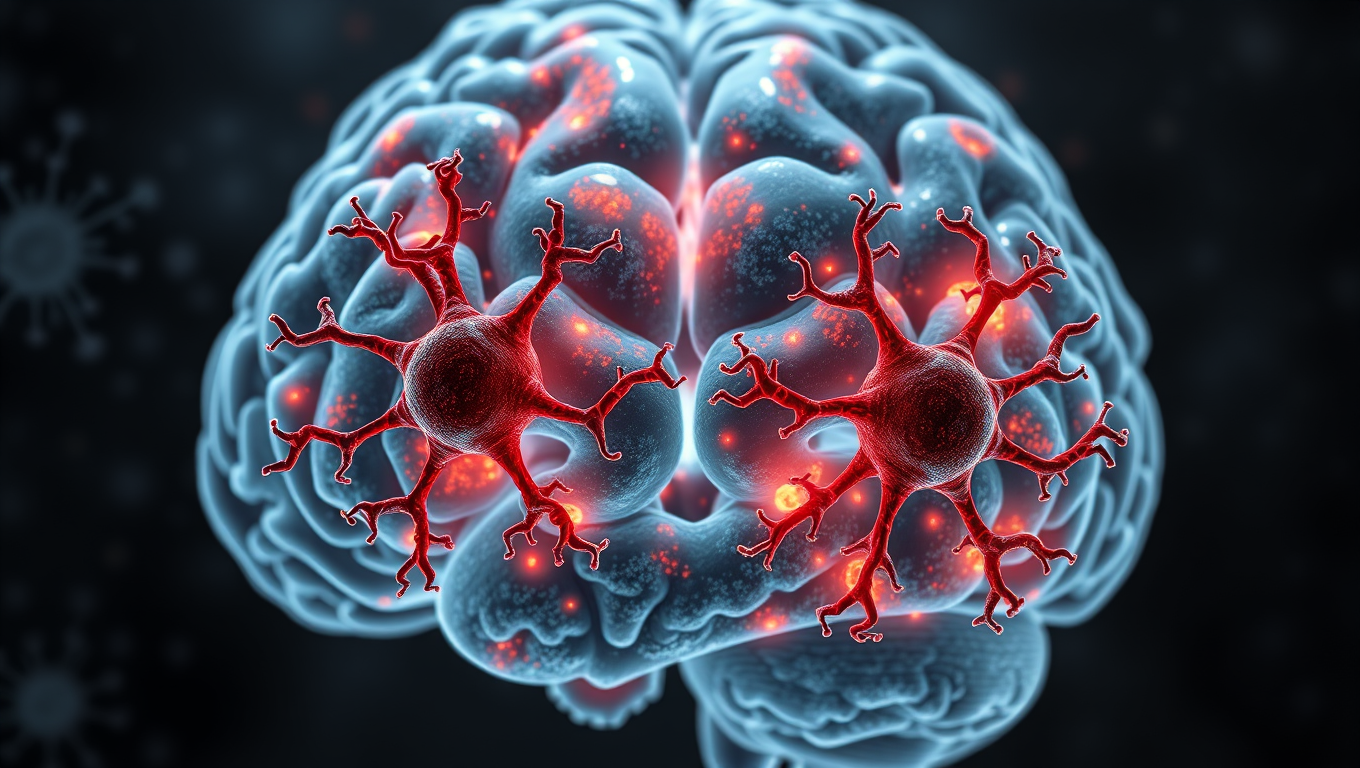
Breaking New Ground: Immune System Discovery Offers Potential Solution to Alzheimer’s
A new way of thinking about Alzheimer’s disease has yielded a discovery that could be the key to stopping the cognitive decline seen in Alzheimer’s and other neurodegenerative diseases, including ALS and Parkinson’s.
Alzheimer's
Different Versions of APOE Protein Alter Microglia Function in Alzheimer’s Disease
A new study suggests how APOE2 is protective while APOE4 increases disease risk by regulating the brain’s immune cells.
-

 Detectors10 months ago
Detectors10 months agoA New Horizon for Vision: How Gold Nanoparticles May Restore People’s Sight
-

 Earth & Climate11 months ago
Earth & Climate11 months agoRetiring Abroad Can Be Lonely Business
-

 Cancer11 months ago
Cancer11 months agoRevolutionizing Quantum Communication: Direct Connections Between Multiple Processors
-

 Albert Einstein11 months ago
Albert Einstein11 months agoHarnessing Water Waves: A Breakthrough in Controlling Floating Objects
-

 Chemistry11 months ago
Chemistry11 months ago“Unveiling Hidden Patterns: A New Twist on Interference Phenomena”
-

 Earth & Climate11 months ago
Earth & Climate11 months agoHousehold Electricity Three Times More Expensive Than Upcoming ‘Eco-Friendly’ Aviation E-Fuels, Study Reveals
-

 Agriculture and Food11 months ago
Agriculture and Food11 months ago“A Sustainable Solution: Researchers Create Hybrid Cheese with 25% Pea Protein”
-

 Diseases and Conditions11 months ago
Diseases and Conditions11 months agoReducing Falls Among Elderly Women with Polypharmacy through Exercise Intervention