While we try to keep things accurate, this content is part of an ongoing experiment and may not always be reliable.
Please double-check important details — we’re not responsible for how the information is used.
Chronic Illness
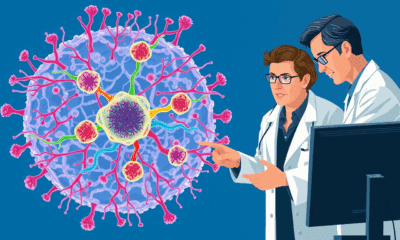
A New Target for Lyme Disease Treatment: Researchers Discover Achilles Heel of Borrelia Burgdorferi
Researchers have discovered that an enzyme can serve as an ideal target for developing new therapeutics against Lyme disease, and most likely other tick-borne diseases as well.

Alternative Medicine
“The Power of Movement: How Regular Exercise Can Add Years to Your Life”
Adopting a physically active lifestyle at any stage of adulthood significantly lowers your risk of dying from any cause, especially from cardiovascular disease. A sweeping analysis of 85 studies confirms that those who stay active consistently reduce their mortality risk by 30–40%, while even those who become active later in life enjoy a 20–25% reduction.
Animals
The Lemur Secret to Aging without Inflammation: A Breakthrough for Human Health?
What if humans didn’t have to suffer the slow-burning fire of chronic inflammation as we age? A surprising study on two types of lemurs found no evidence of “inflammaging,” a phenomenon long assumed to be universal among primates. These findings suggest that age-related inflammation isn’t inevitable and that environmental factors could play a far bigger role than we thought. By peering into the biology of our primate cousins, researchers are opening up new possibilities for preventing aging-related diseases in humans.
Chronic Illness
The Surprising Link Between Hearing Loss, Loneliness, and Lifespan
People who treat hearing loss with hearing aids or cochlear implants regain rich conversations, escape isolation, and may even protect their brains and lifespans—proof that better hearing translates into fuller living.
-

 Detectors3 months ago
Detectors3 months agoA New Horizon for Vision: How Gold Nanoparticles May Restore People’s Sight
-

 Earth & Climate4 months ago
Earth & Climate4 months agoRetiring Abroad Can Be Lonely Business
-

 Cancer4 months ago
Cancer4 months agoRevolutionizing Quantum Communication: Direct Connections Between Multiple Processors
-

 Agriculture and Food4 months ago
Agriculture and Food4 months ago“A Sustainable Solution: Researchers Create Hybrid Cheese with 25% Pea Protein”
-

 Diseases and Conditions4 months ago
Diseases and Conditions4 months agoReducing Falls Among Elderly Women with Polypharmacy through Exercise Intervention
-

 Albert Einstein4 months ago
Albert Einstein4 months agoHarnessing Water Waves: A Breakthrough in Controlling Floating Objects
-

 Chemistry4 months ago
Chemistry4 months ago“Unveiling Hidden Patterns: A New Twist on Interference Phenomena”
-

 Earth & Climate4 months ago
Earth & Climate4 months agoHousehold Electricity Three Times More Expensive Than Upcoming ‘Eco-Friendly’ Aviation E-Fuels, Study Reveals